March 29, 2023 -- Expansion of a diverse subset of T-cell clones influences how patients respond to immune checkpoint inhibitors (ICIs), suggesting it may be possible to predict who will benefit from the treatments.
ICIs such as Merck's Keytruda have transformed the treatment of a range of tumor types by turning the immune system against cancer cells. However, while ICIs are highly effective in a subset of patients, most people do not respond to the treatments. The low response rates have created a need for ways to identify who the drugs will benefit, thereby sparing people from ineffective treatments, and to bring the benefits of ICIs to more patients.
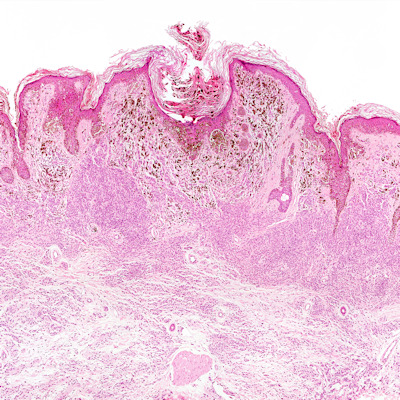
Writing in Cancer Immunology Research, scientists at Tokyo University of Science and The University of Tokyo outline their work to understand the factors that dictate whether a patient responds to an ICI. The study focused on the correlation between antitumor effects and CD8+ tumor-infiltrating T-lymphocytes (TIL) clones.
TILs are the primary effector cells that lead to antitumor response and are composed of various T-cell clones that are determined by their unique T-cell receptor (TCR) genes. Earlier work has shown that TCR diversity can indicate that a TIL population can recognize multiple tumor antigens, but knowledge of the mechanistic link between the diversity of tumor-reactive clones influences and health outcomes was lacking.
To fill the knowledge gap, the Tokyo researchers analyzed the TCR repertoire of two mouse models after treatment with ICIs. The analysis showed that the treatments increased the mobilization of overlapping (OL) T-cell clones in draining lymph nodes (dLNs) and tumors.
Categorization of the dLN-tumor OL clones into oligoclonal and polyclonal fractions shed further light on the process. Unlike oligoclonal clones, polyclonal clones are derived from two or more cells of different ancestry or genetic constitution. Separating the two sets of clones showed ICIs significantly increased the polyclonal fraction of OL repertoire without changing the oligoclonal fraction.
The findings suggest the expansion of diverse polyclonal clones, a process known as clonal spreading, is central to the response to ICIs. Associate professor Satoshi Ueha, one of the authors of the paper, described what the findings could mean for the treatment of cancer.
"Our results can be used to predict and diagnose the efficacy of ICIs, thereby making it possible to deliver these rather expensive drugs to patients who can benefit from them. In the long term, the clonal spreading response found in our study may be used to develop therapeutic drugs that induce stronger anti-tumor T-cell responses when used in combination with ICIs," Ueha said in a statement.
Copyright © 2023 scienceboard.net