May 15, 2023 -- Toronto's University Health Network (UHN) neurosurgeons have developed a novel glioblastoma therapy that combines the injection of an oncolytic virus directly into the tumor with intravenous immunotherapy. The results, published Monday in Nature Medicine, found that this combination therapy prolonged survival rates, providing clinical benefits to over half of the patients studied.
Glioblastoma is a notoriously difficult-to-treat primary brain cancer. Despite aggressive treatment, which typically involves surgical tumor removal and multiple chemotherapy drugs, the cancer often returns, at which point treatment options are limited.
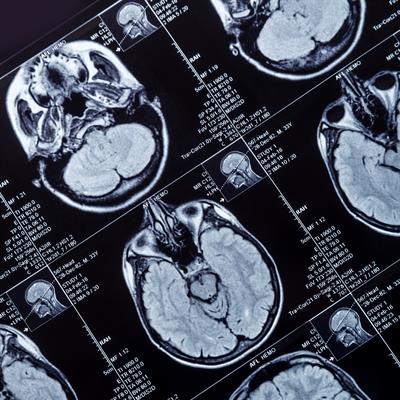
The team evaluated their combination therapy in a phase I/II clinical trial testing the safety, side effects, and best dose of new treatments. They recruited 49 patients with recurrent disease, who did not have tumor resection at recurrence, from 15 hospital sites across North America.
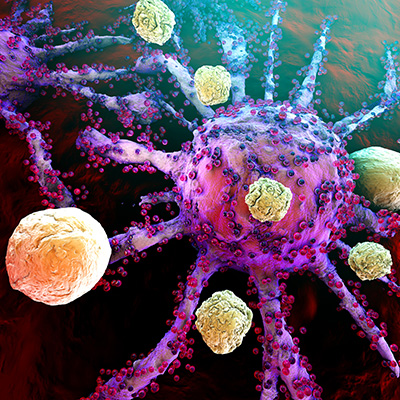
Using stereotactic techniques, the team first accurately localized the tumor, then directly injected the oncolytic virus through a small hole with a purpose-built catheter. Oncolytic viruses -- viruses that target and kill cancer cells -- create more favorable tumor microenvironments, which helps boost antitumor immune responses. Patients then received an intravenous anti-PD-1 antibody called pembrolizumab as targeted immunotherapy every three weeks, starting one week after surgery.
The combination of the oncolytic virus and immune-checkpoint inhibition resulted in a "double hit" to tumors; the virus directly caused cancer cell death, but also stimulated local immune activity, leaving the cancer cells more vulnerable to targeted immunotherapy.
The combination therapy was found to be safe, well tolerated, and life-extending, yielding a median survival of 12.5 months compared with the six to eight months typically achieved with existing therapies. Over half the patients achieved disease stability or better; some tumors shrank or were eradicated. Three patients remained alive at 45, 48, and 60 months after starting the clinical trial.
The team also performed experiments to define the mutations, gene expression, and immune features of each patient's tumor. They discovered a new genetic signature within tumor samples that may enable better understanding of glioblastoma resistance mechanisms, and potentially predict which glioblastoma patients are most likely to respond to treatment.
The researchers believe delivering the virus directly into the tumor prior to using systemic immunotherapy was key to their success, and that a subpopulation of glioblastoma patients will respond well to this treatment. Their study represents one of the few clinical trials over the last decade with favorable results for glioblastoma.
Next steps will involve testing the combination therapy's effectiveness against other treatments in a randomized clinical trial. The researchers believe that translational work, combining basic science with clinical trials, is key to moving personalized glioblastoma treatments forward.
"We are encouraged by these results, but there is still a lot of work ahead of us," first author Dr. Farshad Nassiri, a UNH neurosurgeon, said in a statement. "Our goal, as always, is to help our patients. That's what motivates us to continue this research."
Copyright © 2023 scienceboard.net