December 8, 2022 -- An analysis of T-cell receptors (TCRs) by researchers at the Washington University School of Medicine, and colleagues at Stanford University and Oxford University, has generated evidence that microbial antigens and self-antigens could play a pathogenic role in certain autoimmune diseases.
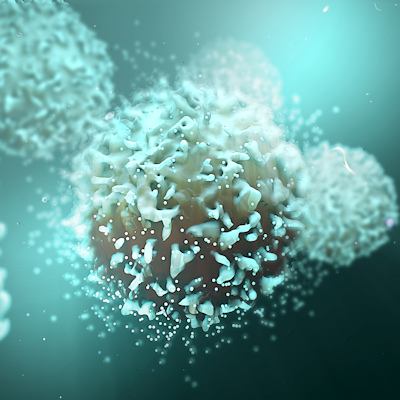
The study, details of which were published December 7 in the journal Nature, was designed to help clear up the question of how autoimmune diseases develop. In people with autoimmune diseases, immune cells -- which should only go after pathogens -- attack healthy tissues. The diseases are thought to arise when the immune system mistakes a human protein for a pathogenic protein, but the specific proteins have proven elusive.
In some inflammatory diseases of the spine, pelvis, and eye, such as ankylosing spondylitis and acute anterior uveitis, human leukocyte antigen B*27 (HLA-B*27) may play a role but the specific mechanism is unknown. The mechanism may involve the presentation of pathogenic peptides to CD8+ T cells.
To explore that idea, researchers isolated orphan TCRs expressing a disease-associated motif from the blood and synovial fluid T cells of individuals with ankylosing spondylitis and from the eyes of people with acute anterior uveitis. Analyzing the TCRs revealed consistent features and showed clonal expansion in the joint and eye.
Stanford University School of Medicine's K. Christopher Garcia, PhD, co-corresponding author of the Nature paper, outlined the significance of the study's findings -- and the approach that enabled them -- in a statement.
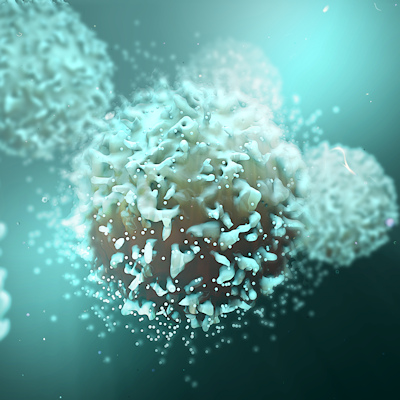
"This study reveals the power of studying T cell specificity and activity from the ground up; that is, identifying the T cells that are most active in a given response, followed by identifying what they respond to," Garcia said. "Clearly these patient-derived TCRs are seeing a spectrum of common antigens, and that may be driving the autoimmunity. Proving this in humans is very difficult, but that is our future direction and could lead to therapeutics."
Garcia and his collaborators showed that T cells in the joint and eye, the sites of pathology for the two studied diseases, recognize HLA-B*27 bound to both self and microbial antigens. The finding could lead to improved treatments, as Garcia noted, by revealing disease-causing T cells that can be targeted for elimination, and potentially to new diagnostics that enable more timely interventions.
On average, almost eight years pass between the appearance of the first symptoms of ankylosing spondylitis and the correct diagnosis of the autoimmune condition. If a diagnostic test shortens the time to diagnosis, it could enable physicians to intervene before the disease progresses and thereby improve outcomes.
"As for therapeutics, if we could target these disease-causing T cells for elimination, we could potentially cure a patient or maybe even prevent the disease in people with the high-risk genetic variant. There's a lot of potential for clinical benefit here," said co-first author Dr. Michael Paley, PhD, an assistant professor at Washington University.
Copyright © 2022 scienceboard.net