July 8, 2022 -- A small subset of the CAR T cells prepared for therapy produce most of the anticancer activity, suggesting it may be possible to improve the treatment.
In a study published on July 6 in the journal Cancer Discovery, researchers described the identification of a genetic signature on pre-infusion CAR T cells that became the cancer-killing effector T cells.
Sorting CAR T cells by the surface markers could limit infusions to cells that will go on to become effector T cells, although the researchers caution the signature may only apply to certain cancer types.
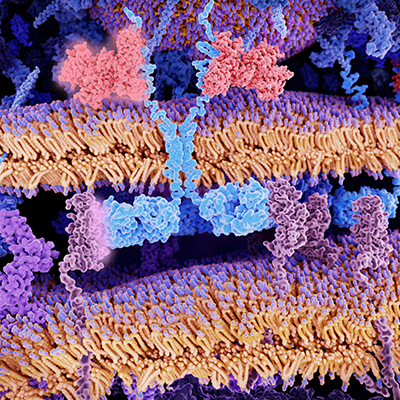
Currently, CAR T cell products are evaluated in bulk. The St. Jude Children's Research Hospital team behind the study questioned if assessing functional heterogeneity could improve CAR T outcomes, leading to the creation of a single-cell gene expression and T-cell receptor (TCR) sequencing dataset. The dataset used pre- and post-infusion CD19-CAR T cells from pediatric patients with B cell acute lymphoblastic leukemia.
Because each T-cell lineage has a unique TCR, the researchers were able to use the protein as a barcode for identifying cells from the same source. The team sequenced the TCRs in the pre-infusion cells and in patient samples after therapy and used machine learning to see if cells later became effector T cells.
Through the analysis, the researchers revealed a pre-effector signature possessed by a small proportion of cells. Specifically, the team identified three genes within the signature that encode for proteins found on the surface of the T cell. If a cell had that combination of surface proteins, they became effector T cells. The cells without the combination of surface proteins became "dysfunctional."
"It was a surprising finding," Paul Thomas, PhD, co-corresponding author of the study, said in a statement. "It appears that a very small proportion, certainly the minority of CAR positive T cells in the pre-infusion product, are actually contributing to the antitumor response in the patient."
The "unexpected surface phenotype" of the pre-effector cells was TIGIT+, CD62Llo, and CD27-. The finding suggests a refined version of the method could identify cells with the pre-effector signature before they are infused, enabling the enrichment of the therapy with cells that are most likely to mount an effective attack against the cancer.
One outstanding question is whether the signature is found outside of the studied cells. It is possible that the cell surface markers are unique to the combination of CAR T cell, cancer, and patient population studied in the Cancer Discovery paper.
Copyright © 2022 scienceboard.net