November 18, 2022 -- A macrocyclic cell-penetrating peptide conjugate has enabled a cisplatin prodrug to cross the blood-brain barrier (BBB) in mice, increasing survival rates and providing a potential pathway for treating humans with brain cancer.
The BBB stops most drugs from entering the brain and thereby makes it hard to treat conditions such as glioblastoma (GBM), the most aggressive primary malignant brain tumor. Researchers have proposed a range of ways of getting molecules across the barrier, such as direct intraventricular injection, implants that release the drug, and the use of focused ultrasound to temporarily open the BBB.
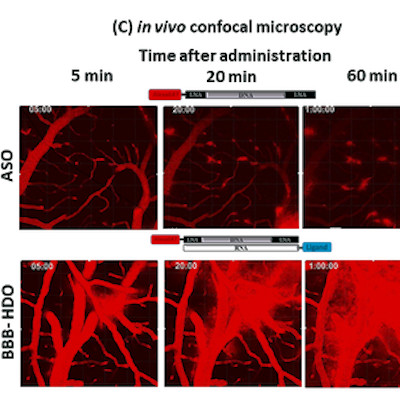
Another avenue of research focuses on using BBB-penetrant nanoparticles, liposomal formulations, and peptide-based delivery systems to hustle drug molecules across the barrier. A team at Brown University previously contributed to the literature on that approach by reporting the synthesis of a BBB-penetrant macrocyclic cell-penetrating peptide conjugate (M13) covalently linked to a Pt(IV) cisplatin prodrug.
Published online in advance of the December issue of the Journal of Controlled Release, the researchers shared details of the next step in their work on the Pt(IV)-M13 conjugate. The paper describes an in vitro study that showed the conjugate releases active cisplatin, a platinum-based chemotherapy drug, upon intracellular reduction and causes the death of GBM cells.
Encouraged by the in vitro data, the team studied the effect of intravenous delivery of the Pt(IV)-M13 conjugate in mice with GBM tumors. The in vivo assessment linked the conjugate to higher levels of platinum in the brain and tumor than was achieved by cisplatin alone. Similarly, the conjugate was better tolerated than cisplatin and significant extended survival.
Median survival in mice that received the Pt(IV)-M13 conjugate was 33 days, compared to between 22 days and 24 days for mice that received either the Pt(IV) prodrug, cisplatin or the control. Jorge Jimenez Macias, an author of the study and postdoctoral fellow at Brown, explained the importance of the study in a statement.
"This new technology allowed us to test drugs against brain cancer that previously hadn't been used against glioblastoma because they hadn't been able to cross the blood-brain barrier. We have shown for the first time that the linking of an anticancer drug to a macrocyclic cell-penetrating peptide leads to effective dosing in mice at many times higher than the drug alone, which can significantly extend survival," Jimenez Macias said.
The collaborators believe they can improve the treatment and survival rate "quite significantly" through further optimization and tweaking of the drug and delivery system.
Copyright © 2022 scienceboard.net