April 24, 2023 -- Early tests show that a bioengineered drug can counter infection with Staphylococcus aureus, a major cause of death in hospital patients. The research, published Monday in Cell Host & Microbe, demonstrated that the antibacterial biologic agent was superior to standard antibiotic drugs at treating S. aureus-infected mice, including its treatment-resistant form methicillin-resistant Staphylococcus aureus (MRSA).
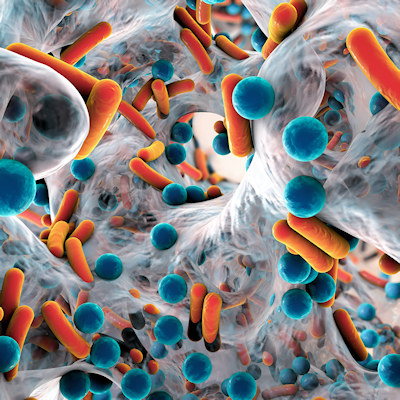
One-third of all people are asymptomatic S. aureus carriers, but those with weakened immune systems may develop life-threatening lung, heart, bone, or bloodstream infections, especially when hospitalized.
The researchers investigated the multivalent human antibody-centyrin fusion protein mAbtyrins, a combination molecule based on an engineered version of a human monoclonal antibody (mAb); mAb proteins cling to and mark S. aureus for uptake and destruction by immune cells. Attached to mAbs are centyrins, small proteins that prevent the bacteria from boring holes into the immune cells.
The treatment targets disease-causing mechanisms employed by S. aureus without killing it. This approach better addresses antibiotic resistance, in which antibiotics kill vulnerable strains first, making more space for other less-vulnerable strains until the drugs no longer work.
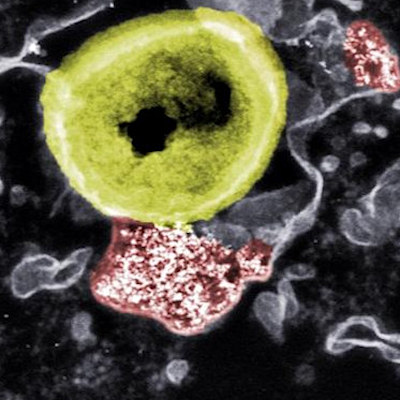
The team fused centyrins to a mAb taken from a patient recovering from S. aureus infection. Primed by its bacterial encounter, the mAb labeled the bacterial cells so that they were pulled into bacteria-destroying pockets inside roving immune cells called phagocytes.
However, the team needed to prevent the toxins that enable S. aureus to drill into immune cells from the outside from drilling out of the pockets from the inside. Therefore, part of the bioengineered mAbtyrin serves as a "passport" recognized by immune cells, which then engulf the entire bacteria, along with the attached mAbtyrin and its centyrins, and fold it into pockets. Once inside, the centyrins block the bacterial toxins, setting this drug apart from antibody combinations that target toxins only outside of cells.
In the lab, researchers found that bacterial populations grew slightly less normally in the presence of their engineered mAb, and only half as fast when mAbtyrin was used. Of mice infected with S. aureus and treated with a control mAb without centyrins, 98% developed bacteria-filled kidney sores, while only 38% of mice treated with mAbtyrin did so. When bacteria colonies were counted, tissues from mice treated with mAbtyrin had 100 times fewer bacterial cells than those treated with a control mAb.
Finally, small doses of the antibiotic vancomycin -- a last line of defense against MRSA -- administered in combination with mAbtyrin in mice significantly improved mAbtyrin's efficacy, resulting in maximum reduction of bacterial loads in kidneys and 70% protection from kidney lesions.
"This is the first report showing that mAbtyrins can drastically reduce populations of this pathogen in cell studies, and in live mice infected with drug-resistant strains so common in hospitals," Dr. Victor Torres, lead author and a New York University microbiology professor, said in a statement. "Our goal was to design a biologic that works against S. aureus inside and outside of cells, while also taking away the weapons it uses to evade the immune system."
Disclosure: This work was supported by Janssen Biotech. Dr. Torres has recently received royalties and consulting compensation from Janssen.
Copyright © 2023 scienceboard.net