April 19, 2023 -- The U.S. Food and Drug Administration (FDA) on Monday approved the product Omisirge, a cell therapy treatment, for transplantation in blood cancer patients. The phase III trial results, published October 21, 2021, in the journal Blood, found the efficacy of Omisirge transplantation superior to standard umbilical cord blood transplantation.
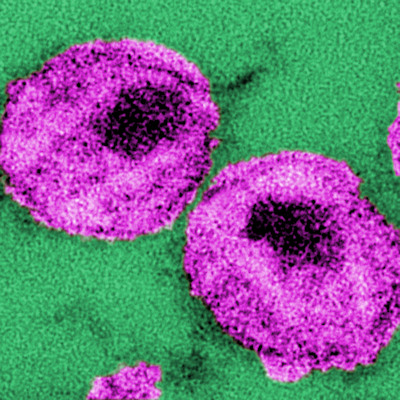
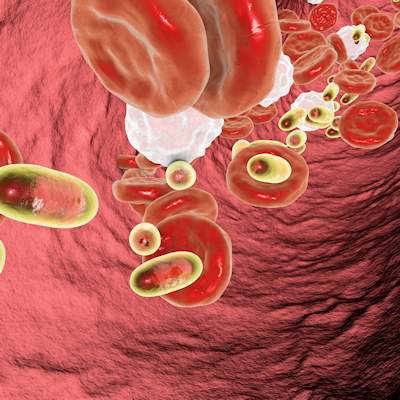
Blood cancers, which represent about 10% of all U.S. cancer cases, occur when abnormal blood cells begin proliferating, disrupting the normal blood cells' ability to perform essential functions. Blood cancers, including leukemia, lymphoma, and myeloma, can cause serious symptoms, including fatigue, bone and joint pain, infections, weakness, weight loss, and fever; they can also be fatal.
Umbilical cord blood transplantation is a common blood cancer treatment. It involves putting healthy stem cells into the body to restore the blood's normal function. Prior to transplantation, patients often undergo radiation or chemotherapy to kill off their dysfunctional blood cells. Since this process weakens the immune system, severe and sometimes deadly infections are a frequent risk.
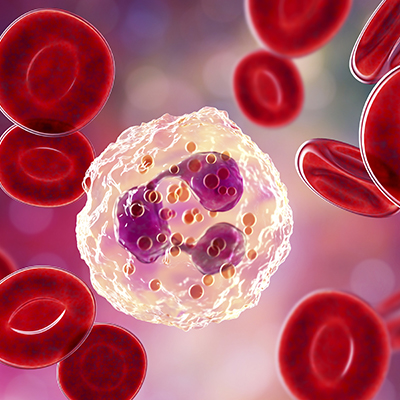
Omisirge (omidubicel-onlv), created by Israel-based biotech Gamida Cell, is a single-dose therapy administered intravenously to hasten the recovery of neutrophils -- a type of white blood cell -- and reduce the risk of post-transplant infection. It is made up of donor stem cells from umbilical cord blood that are processed with nicotinamide, a form of vitamin B3, and intended for blood-cancer patients ages 12 and older.
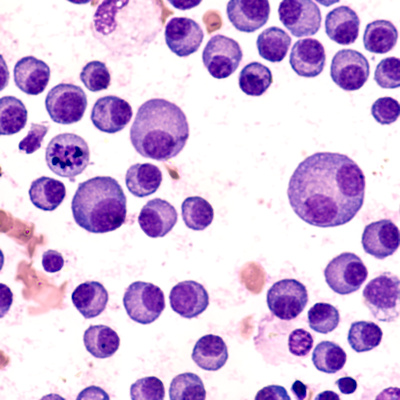
The safety and effectiveness of Omisirge was supported by a randomized, multicenter study enrolling 125 patients with confirmed blood cancers between 12 and 65 years of age. Omisirge's efficacy was based on the amount of time needed for neutrophil recovery, and the incidence of infections following transplantation.
Of patients randomized to receive Omisirge, 87% achieved neutrophil recovery within a median of 12 days following treatment with the product, compared to 83% who received umbilical cord blood transplantation and achieved neutrophil recovery within a median of 22 days. Bacterial or fungal infections within 100 days after transplantation were seen in 39% of patients receiving Omisirge, versus 60% of those in the control group who received umbilical cord blood. However, researchers caution that Omisirge treatment may cause severe side effects including infections, graft versus host disease, and infusion reactions, and less commonly, engraftment syndrome, graft failure, and secondary malignancies.
Omisirge has received FDA breakthrough therapy designation, priority review, and orphan drug designation, reflecting an unmet need for additional donor sources for stem cell transplantation. More than 40% of the study's patients were racially and ethnically diverse, underscoring the degree to which Omisirge may help address stem cell transplantation health disparities.
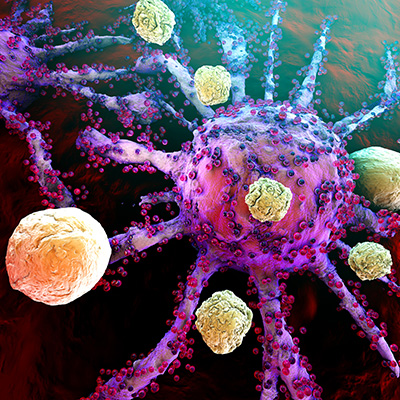
"Hastening the return of the body's white blood cells can reduce the possibility of overwhelming infection associated with stem cell transplantation," Dr. Peter Marks, director of the FDA's Center for Biologics Evaluation and Research, said in a statement. "This approval is an important advance in cell therapy treatment in patients with blood cancers."
Copyright © 2023 scienceboard.net