February 9, 2023 -- Researchers have discovered that tiny gene fragments called microexons are prevalent in pancreatic islets – tissues that host beta cells which produce insulin. The findings, published February 9 in Nature Metabolism, indicate that microexons may constitute new therapeutic targets for diabetes treatment.
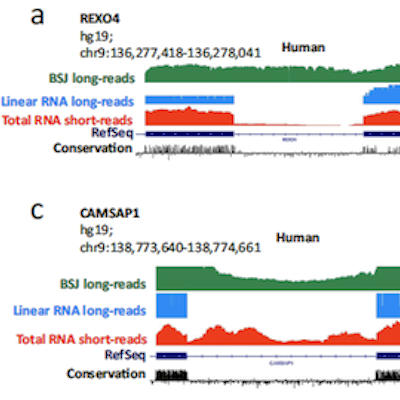
When cells copy DNA to produce RNA transcripts, they include specific chunks of genetic material called exons, resulting in RNA molecules used as protein-building templates. However, recently discovered protein-coding DNA sequences much shorter than exons, called microexons, have been conserved across different species for millions of years, suggesting their important function.
Growing evidence suggests that microexons play crucial roles in human development, health, and disease. In humans, most microexons are exclusively found in neuronal cells, where the tiny gene fragments exert an outsized role, including the development of photoreceptor neurons in the retina. Microexon activity alterations are also common in autistic brains.
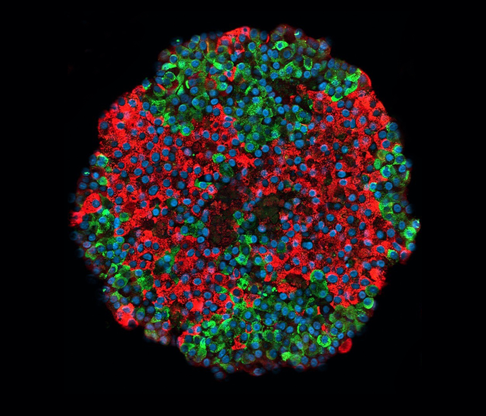
Researchers have now discovered that half the exons specifically enriched in pancreatic islets are microexons. Almost all are also found in neuronal cells -- suggesting that pancreatic islet cells evolved by borrowing regulatory mechanisms from neuronal cells. Of over 100 pancreatic islet microexons found, the majority were located on genes critical for insulin secretion or linked to type-2 diabetes risk. Microexon inclusion in RNA transcripts was controlled by SRRM3, a protein that binds to RNA molecules and is encoded by the SRRM3 gene. High blood sugar levels, induced both by SRRM expression and the inclusion of microexons, indicate that microexon splicing regulation plays a role in maintaining blood sugar levels.
Performing experiments using laboratory-grown human beta cells, as well as mice lacking the SRRM3 gene, researchers found that depleting SRRM3 or repressing single microexons lead to impaired insulin secretion in beta cells. In mice, alterations to microexon splicing changed the shape of the pancreatic islets, ultimately impacting insulin release.
Studying genetic and RNA transcript data from diabetic and nondiabetic individuals, researchers found that genetic variants affecting microexon inclusion are linked to variations in fasting blood sugar levels and type-2 diabetes risk. Type-2 diabetes patients were also found to have lower levels of microexons in their pancreatic islets. Due to their potential contribution to type-2 diabetes predisposition, researchers say microexons may represent ideal therapeutic targets to treat dysfunctional beta cells in type-2 diabetes.
"Less than 10 years after we first reported on their existence, we are seeing how microexons are key elements that modify how proteins interact with each other in cells with functions that require a high degree of specialization, such as neurotransmitter or insulin release and light transduction," explained Centre for Genomic Regulation co-author Dr. Manuel Irimia in a statement. "Consequently, we expect mutations in microexons to lead to diseases whose genetic causes we have not yet understood. We are beginning to search for these mutations in patients with neurodevelopmental and metabolic disorders as well as retinopathies, to then devise possible interventions to treat them."
Copyright © 2023 scienceboard.net