March 31, 2022 -- Using bacteria to target tumors is a promising avenue for developing new treatments, although the risk of severe side effects is holding back clinical trials. Now, in a new study published on March 17 in Nature Biotechnology, researchers have developed a way to reversibly hide the microbes from the immune system, providing control over their growth.
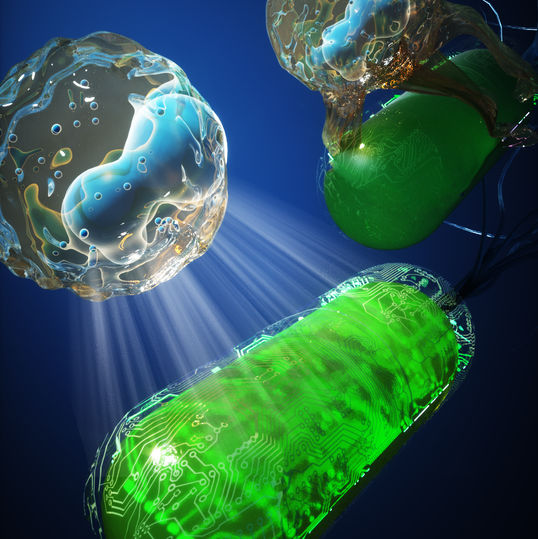
The medical community's war on cancer has produced a wide range of therapies, including keyhole surgery, precision radiation, toxic chemicals, targeted proteins, and manipulated immune cells. And in the future, we might be able to add bacteria to that growing list. Engineered as living medicines, they can grow, spread, and deliver toxic payloads into cancerous tissue.
Using bacteria to treat cancer is not a new idea. In the late 19th century, surgeon William Coley injected live microbes into patients with inoperable cancers. However, the approach did not take off as it presented considerable risk and other doctors failed to replicate his results.
One of the main downsides of this approach is the response from the human immune system. Our cellular sentinels are quick to respond to signs of an infection and will either wipe out the bacteria before they can be effective or trigger severe inflammation in an attempt to fight them. This makes it extremely difficult to find a suitable dosage that is reliably safe and effective. Recent clinical trials to test live bacteria therapy had to be stopped due to toxicity at low doses.
Temporary evasion
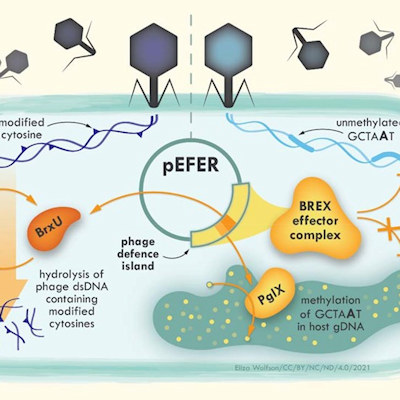
To get around this problem, researchers at Columbia University have created a system that allows them to control the immune response. This is based on chains of sugars known as capsular polysaccharide (CAP), which many bacteria have on their surface to protect them from environmental conditions. Inside the human body, CAP acts as an invisibility cloak to shield "friendly" probiotic bacteria from the immune system and allows them to survive and grow.
"With CAP, these bacteria can temporarily evade immune attack; without CAP, they lose their encapsulation protection and can be cleared out in the body. So, we decided to try to build an effective on/off switch," said Tetsuhiro Harimoto, the lead author of the paper, in a statement.
After identifying the gene responsible for CAP in a probiotic strain of E. coli, the team created a synthetic version that they could activate by adding a small molecule called isopropyl-b-D-thiogalactopyranoside (IPTG). When the IPTG is removed, the protection from CAP is stripped away and the E. coli bacteria are left vulnerable.
This approach, which the researchers called inducible CAP or iCAP, allowed the scientists to directly manage the growth of the engineered bacteria. By varying the amount of IPTG present, they could alter how long the modified microbes survived in samples of human blood.
"Bacterial cancer therapy holds unique advantages over conventional drug therapy, such as efficient targeting of the tumor tissue and programmable drug release. Potential toxicity has been limiting its full potential. The cloaking approach presented in this study may address this critical issue," said Kam Leong, PhD, professor of biomedical engineering at Columbia University.
Targeting tumors
The team tested the system in mice by injecting the modified E. coli into the bloodstream and found that the mice could tolerate ten times the dose compared to normal bacteria. When the E. coli was engineered to produce a cancer-killing toxin, just a single dose given to the mice significantly suppressed the growth of breast and colorectal cancers.
This approach can also target tumors that have spread to other parts of the body. The scientists injected the altered bacteria directly into a tumor in mice and gave them drinking water containing IPTG. Within three days, the bacteria spread to other cancer sites in the body and reduced their growth. Without IPTG, the immune system prevented the microbes from traveling through the bloodstream to reach the other tumors.
"While there is a good deal of laboratory research showing various ways to engineer microbes, it is very difficult to apply these powerful therapies to a complex animal or human body. We've shown proof of concept in mouse models, but given that humans are 250 times more sensitive to bacterial endotoxins than mice, we expect our results may have an even bigger effect on human patients than on mice," said Harimoto.
There are over 80 other distinct CAP systems in E. coli, with many more in other bacterial species, which presents an opportunity to develop and expand this approach further. The researchers also suggest that other control methods could be developed, instead of manually adding IPTG, so that the growth of the microbes could be managed automatically based on physiological conditions.
Copyright © 2022 scienceboard.net