January 19, 2023 -- Researchers have engineered a bacterium that serves as a "living medicine" to treat antibiotic-resistant lung infections -- the leading cause of hospital mortality. The research, published January 19 in the journal Nature Biotechnology and supported through CaixaResearch Health, focused on the antibiotic-resistant bacterium Pseudomonas aeruginosa, a common source of difficult-to-treat hospital infections.
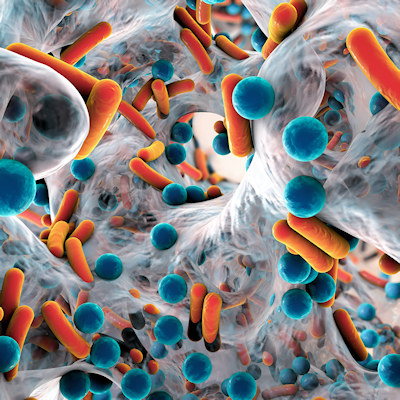
P. aeruginosa lives in communities that form biofilms which can attach to various surfaces in the body, forming impenetrable structures that escape antibiotics. These biofilms can grow on the surface of endotracheal tubes used by critically-ill patients who require mechanical ventilators to breathe. This causes ventilator-associated pneumonia, a condition which affects one in four intubated patients. The incidence exceeds 50% for patients intubated due to severe COVID-19. It can extend the duration in intensive care by 13 days and kills up to one in eight patients.
The "living medicine" treatment uses a modified version of the tiny bacterium Mycoplasma pneumoniae. With only 684 genes and no cell wall, M. pneumoniae's simplicity makes it well-suited for bioengineering for specific applications. Because M. pneumoniae is naturally adapted to lung tissue, it is ideal for respiratory disease treatment. Once administered, the modified bacterium travels to the respiratory infection source, where it sets up shop and produces a variety of therapeutic molecules, including pyocins.
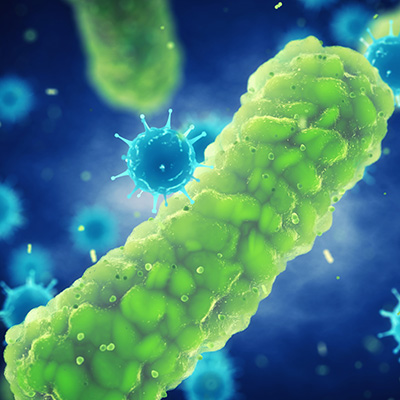
In this study, researchers removed M. pneumoniae's ability to cause disease and repurposed it to attack P. aeruginosa. They found that the treatment acted as a "living medicine," preserving air in the alveoli, and significantly reducing lung infections in mice. Mouse survival rates were doubled compared to mice left untreated. Following treatment, the immune system cleared the modified bacteria in four days. Bioengineered M. pneumoniae can also dissolve biofilms by producing pyocins, toxins that kill or inhibit Pseudomonas growth. Researchers found the treatment successfully dissolved P. aeruginosa biofilms collected from the endotracheal tubes of patients in intensive care units.
The researchers hope to eventually conduct clinical trials, and potentially use this "living medicine" in nebulizers to treat ventilator-associated pneumonia. They say the bacterium can potentially be modified with a variety of different payloads, including cytokines, nanobodies, or defensins. Their aim is to diversify the modified bacterium's arsenal and unlock its full potential in treating a variety of complex diseases. The study may also open doors for creating new strains of the bacteria to treat other respiratory diseases, including lung cancer or asthma.
"We have developed a battering ram that lays siege to antibiotic-resistant bacteria. The treatment punches holes in their cell walls, providing crucial entry points for antibiotics to invade and clear infections at their source. We believe this is a promising new strategy to address the leading cause of mortality in hospitals," said Centre for Genomic Regulation's co-corresponding author María Lluch, PhD, in a statement.
Copyright © 2023 scienceboard.net