April 20, 2023 -- Researchers have used human induced pluripotent stem cells (iPSCs) to overcome a barrier to the supply of a potential treatment for amyotrophic lateral sclerosis (ALS) and retinitis pigmentosa.
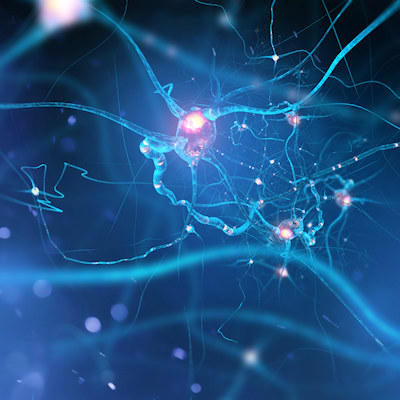
Last year, scientists at Cedars-Sinai Medical Center published early-phase clinical trial data on a potential cell therapy treatment for ALS. The clinical trial studied the effect of cells engineered to produce glial cell line-derived neurotrophic factor (GDNF), a protein that can promote the survival of motor neurons. With the study finding that the treatment is safe, the researchers embarked on further development.
However, supply problems could arise as the one-time treatment moves through the clinic and is needed in larger volumes to meet demand, Clive Svendsen, PhD, executive director of the Cedars-Sinai Board of Governors Regenerative Medicine Institute, explained in a statement.
"The cell lines we are using in the clinic are coming from a single source and are going to eventually run out. We just don't have endless product," said Svendsen. The supply constraints led Svendsen and his collaborators to investigate iPSCs, cells that, because of their strong self-renewal ability, could provide a virtually unlimited source of cells. However, one downside is the potential for iPSCs to cause tumors to develop.
To explore if iPSCs are suitable for their GDNF treatment, the researchers engineered iPSC-derived neural progenitor cells to produce the protein and studied the resulting cell therapy candidates in rodents. The results, which were published on Thursday in Stem Cell Reports, suggest that the approach has potential.
Injecting the cells into the eyes of rodents with retinal degeneration led to protection of the cells in the eye that support vision. Similarly, when transplanted into the spinal cords of rodents with ALS the cells helped protect motor neurons. The cells survived, integrated into the spinal cord, and formed astrocytes, a subtype of glial cells that malfunction in ALS patients.
Importantly, the cells continued to produce GDNF and were safe. No rodents grew tumors or developed other health problems for several months after treatment. The findings led the researchers to conclude that it may be possible to develop human iPSCs that stably produce GDNF to safely provide the benefits of the current clinical trial candidate without the constraints on manufacturing output.
That idea remains unproven. The researchers need to carry out more preclinical tests before moving into human studies, and are exploring ways to improve the expansion of the cells to make the process scale up more easily.
Copyright © 2023 scienceboard.net