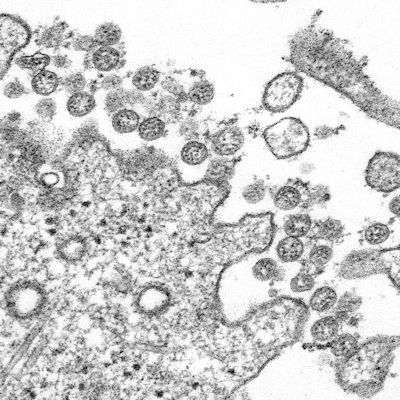
August 12, 2020 -- The SARS-CoV-2 virus can cause the paralysis of key immune cells as the COVID-19 disease progresses, and this immune paralysis can be the difference between severe and mild cases of COVID-19, according to a study published in Science on August 11.
Most COVID-19 patients exhibit mild-to-moderate symptoms, with around 15% progressing to severe or critical disease that requires hospitalization, primarily due to the development of acute respiratory distress syndrome (ARDS). The underlying cause behind the high mortality rate of COVID-19 is unknown but may be due to an impaired interferon response and dysregulated inflammatory responses.
In response to infection with the virus, the body initially launches the rapid -- through somewhat indiscriminate -- innate immune response, followed by a more targeted but slower adaptive immune response. Classifying the dynamic interactions between both types of immune responses and SARS-CoV-2 is an important step in understanding what contributes to the clinical severity of COVID-19 -- and can inform the design of therapeutic strategies.
In the Science paper, researchers used a systems biological approach with mass cytometry and single-cell transcriptomics of leukocytes, transcriptomics of bulk peripheral blood mononuclear cells (PBMCs), and multiplex analysis of cytokines in plasma to analyze the immune response of 76 COVID-19 patients from two geographically distant cohorts.
The Stanford University researchers found an increase in the frequency of plasmablast (immature blood cells that mature into antigen-presenting cells) and effector CD8 T cells in infected individuals. Conversely, there was a decreased frequency of plasmacytoid dendritic cells -- the major producers of type I interferons (IFNs) -- in infected individuals.
The results suggest that patients with COVID-19 may have impaired capacity to produce IFN-alpha. Indeed, they observed reduced production of IFN-alpha in response to stimuli in dendritic cells of infected individuals. This finding suggests that periphery innate immune cells are suppressed during SARS-CoV-2 infection.
Cytokine suspects
Next, the team detected 43 cytokines (including common mediators such as interleukin-6 [IL-6], MCP-3, and CXCL10) that were upregulated in infected samples. This upregulated inflammatory response is despite the impaired interferon response in the blood. The researchers believe that the molecules originate from elsewhere in the body, likely in the lungs at the site of infection.
Three inflammatory mediators were strongly correlated with clinical severity of COVID-19:
- Tumor necrosis factor superfamily member 14 (TNFSF14; LIGHT), expressed in human lung fibroblasts with implications in lung tissue fibrosis, remodeling, and inflammation
- Extracellular newly identified receptor for advanced glycation end products (EN-RAGE), which expresses S100A12, a biomarker of pulmonary injury, and is implicated in pathogenesis of sepsis-induced ARDS
- Oncostatin-M (OSM), a regulator of IL-6
"These three molecules and their receptors could represent attractive therapeutic targets in combating COVID-19," said Bali Pulendran, PhD, senior author of the study and professor of pathology and of microbiology and immunology at Stanford School of Medicine, in a statement. His lab is now testing the therapeutic potential of blocking these molecules in animal models of COVID-19.
Addressing the paradoxical immune paralysis
Lastly, the researchers conducted cellular indexing of transcriptomes and epitopes by sequencing and profiling gene and protein expression in PBMC samples of COVID-19-infected individuals. Clusters of interferon response genes (ISGs) including IFI27, IFITM3, or ISG15 were uniquely associated with COVID-19 patients.
This is a surprising finding, given that innate cells in the blood displayed a reduced ability to produce cytokines. Early on during SARS-CoV-2 infection, low levels of circulating IFN-alpha can be detected, but the effect disappears as disease severity increases.
The study offers a paradox, in which key cells in the innate immune system in the blood of COVID-19 patients become increasingly paralyzed as the disease progresses.
Moreover, the scientists also found elevated levels of bacterial debris, such as bacterial DNA and cell-wall materials, in the blood of those COVID-19 patients with severe cases. The more debris, the sicker the patient -- and the more proinflammatory substances circulating in his or her blood. This could contribute to the immune paralysis caused by SARS-CoV-2.
"One of the great mysteries of COVID-19 infections has been that some people develop severe disease, while others seem to recover quickly," Pulendran explained. "Now we have some insights into why that happens."
Do you have a unique perspective on your research related to virology or immunology? Contact the editor today to learn more.
Copyright © 2020 scienceboard.net