May 11, 2023 -- A CRISPR-based technique has cut the time it takes to create mouse models with mutations that cause cancer, making it easier to show the effects of genetic changes linked to tumor development.
Genomic studies of cancer patients have implicated thousands of genetic mutations in the development of tumors. The studies show that mutations are present in cancer patients but offer no insights into how the genetic changes drive tumorigenesis. Animal models with the genetic changes are needed to show how tumors linked to specific mutations develop in vivo and study how cancer cells respond to treatment.
Researchers have created animal models for some genetic changes by deleting tumor suppressor genes or activating cancer-promoting genes. However, the traditional approach takes months or years to create a model for each mutation. With thousands of mutations to study, the approach is too slow.
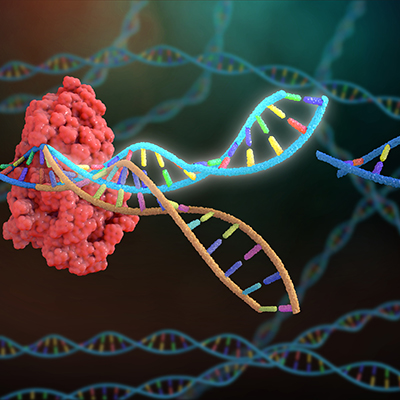
Writing in Nature Biotechnology, researchers at Massachusetts Institute of Technology (MIT) describe a faster way to develop animal models. The study builds on earlier work that showed that CRISPR can quickly and easily knock out genes, but not insert new mutations into a gene, and that a new version of the gene editing technology can make changes by cutting one DNA strand. Traditional CRISPR breaks both strands.
The new version of CRISPR, prime editing, combines a modified Cas9 enzyme with reverse transcriptase. In the new paper, MIT researchers engineered the gene for the prime editor enzyme into the germline cells of mice, causing every cell of the animal to carry a copy. The enzyme enables cells to copy an RNA sequence into DNA that is incorporated into the genome, but it lies dormant until exposed to a protein.
Injecting the protein, Cre recombinase, and a guide RNA that directs Cas9 to make a specific edit into the organ being studied starts tumor growth. The RNA guide can induce single DNA base substitutions, deletions, or additions in a specified gene, allowing the researchers to create any cancer mutation.
The researchers applied the technique to mutations in Kras, a common oncogene. Specifically, the team created animal models of four Kras lung cancer mutations: G12C, G12D, G12R, and G12A. The type of mutation affected tumorigenesis, with G12R producing large, aggressive lung tumors and G12A resulting in smaller, slower-growing cancers. The researchers are now exploring applications of the technique.
"One thing that we're excited about is looking at combinations of mutations including Kras mutations that drives tumorigenesis, along with resistance-associated mutations," Nicolas Mathey-Andrews, an MIT graduate student and co-lead author of the paper, said in a statement. "We hope that will give us a handle on not just whether the mutation causes resistance, but what does a resistant tumor look like?"
Copyright © 2023 scienceboard.net