September 14, 2022 -- Using single-cell sequencing, researchers at the University of Texas MD Anderson Cancer Center have revealed a spatial map of tumor-infiltrating B cells and plasma cells that are prevalent in early-stage lung cancers, providing a basis for finding new immunotherapy targets.
While tumor-infiltrating B and plasma cells are prevalent in lung adenocarcinoma, they are poorly characterized. However, the MD Anderson researchers contend that they have created the largest and most comprehensive single-cell atlas to date on tumor-infiltrating B cells and plasma cells that influence early-stage lung cancer biology and immunotherapy responses.
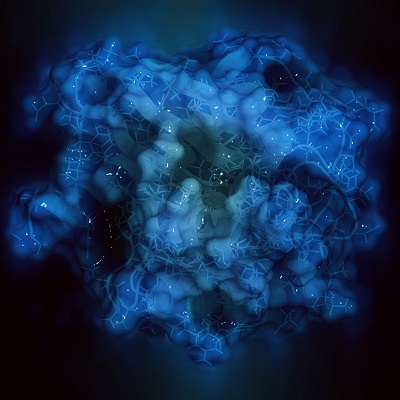
In their study, published September 13 in the journal Cancer Discovery, they describe the use of single-cell RNA and B-cell receptor sequencing of early-stage lung cancers and matching multiregion normal tissues. By analyzing around 50,000 tumor-infiltrating B and plasma cells, the team revealed 12 subsets of cells and showed how they are remodeled in early-stage lung cancer.
The approach enabled the researchers to move past the typical view that tumor-infiltrating B cells or plasma cells are a homogeneous population, as Dr. Linghua Wang, PhD, associate professor of genomic medicine at MD Anderson, explained in a statement.
"Our in-depth analysis highlights the heterogeneous nature of these cells and their crosstalk with other components of the tumor microenvironment," Wang said. "Further studies are needed to fully understand their roles in tumor pathogenesis, but the evidence suggests the plasma cell signature may be a valuable biomarker to predict immunotherapy outcomes. Our findings also can be leveraged to identify new targets for immunotherapy that focus on tumor-infiltrating B cells and plasma cells."
Wang and her collaborators found that memory B cells and plasma cells were highly enriched in tumor tissues "with more differentiated states and increased frequencies of somatic hypermutation." Samples from smokers had "markedly elevated" levels of plasma cells "with distinct differentiation trajectories." The diversity of B-cell receptor clonotype increased in lung cancer, smokers, and as the pathologic stage of the cancer increased, while the same factors were associated with decreased clonality.
Digging deeper, the team showed that lung tumors with epidermal growth factor receptor (EGFR) mutations had lower levels of plasma cells and higher levels of less-differentiated B cells than those with KRAS or other mutations. Combining the single-cell data with spatial information from the tumors, the researchers found tumor-infiltrating B cells and plasma cells were mostly found within lymphoid aggregates with high levels of CXCL13. Production of the CXCL13 chemokine evolved with cancer progression.
The research, which was supported by Johnson & Johnson and the National Institutes of Health, will act as a foundation for further studies intended to clarify the precise roles B cells and plasma cells play in early lung tumor progression. The MD Anderson researchers also plan to identify the most promising therapeutic strategies based on the new knowledge.
Copyright © 2022 scienceboard.net