June 29, 2022 -- Deleting a proinflammatory gene in the beta cells of pre-diabetic mice stops the development of type 1 diabetes, pointing to a potential way to prevent the condition.
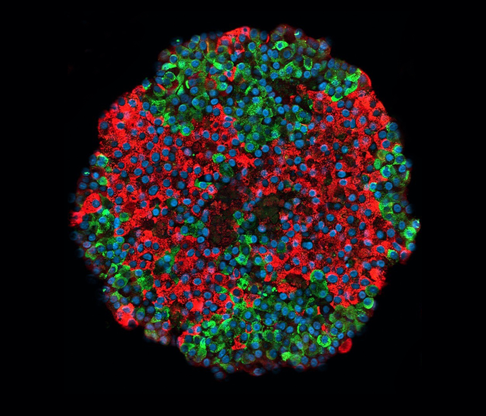
The researchers, who published their findings in the journal Cell Reports, deleted the gene encoding 12/15-lipoxygenase (Alox15), triggering the preservation of beta cell mass, the reduction of populations of infiltrating T cells, and protection against spontaneous autoimmune diabetes.
Based on the findings, the researchers think it may be possible to use therapies targeted at beta cells to stop disease progression, provided the treatment is administered before destruction of the cells has occurred.
The research grew out of an interest in what causes the immune system to destroy pancreatic islet beta cells and, in doing so, drive the pathogenesis of type 1 diabetes. Most research looks at the autoimmune response. The authors of the Cell Reports paper wanted to understand if the beta cells do anything to trigger the autoimmune response that leads to their destruction.
Other teams have linked the enzyme encoded by Alox15, 12/15-LOX, to processes that damage beta cells and generated evidence that it may regulate inflammatory macrophages that initiate attacks on the cells. To build on those findings, the authors of the Cell Reports paper analyzed the role of Alox15 using mouse models.
The researchers backcrossed mice onto the NOD/ShiLtJ background using speed congenics provided by Jackson Laboratories, and then crossed two sets of mice to generate breeding colonies. Treatment of the conditional mice with tamoxifen at 6 weeks old induced deletion of Alox15 in islets. Subsequent tests showed the treatment led to an 80% drop in Alox15 mRNA expression in islets isolated from conditional knockout mice in a process involving collagenase, dissociation in Hank's balanced saline solution (HBSS) and centrifugation.
Using the mice, the researchers showed that deletion of Alox15 reduces beta cell inflammation and stress, protects against spontaneous diabetes development, and alters crosstalk with the immune system. Senior author Dr. Raghavendra Mirmira, PhD, a professor at the University of Chicago, set out the implications of the findings.
"When we got rid of this gene, the beta cells no longer signaled to the immune system and the immune onslaught was completely suppressed, even though we didn't touch the immune system," Mirmira said in a statement. "That tells us that there is a complex dialogue between beta cells and immune cells, and if you intervene in that dialogue, you can prevent diabetes."
The researchers linked loss of Alox15 to increased levels of programmed cell death ligand 1 (PD-L1) in beta cells. Delivering an antibody against PD-L1, an immune checkpoint known for its role in cancer treatments, recovered the diabetic phenotype in knockout mice. Using a drug to increase levels of PD-L1 could prevent the development of diabetes.
Copyright © 2022 scienceboard.net