April 21, 2023 -- Researchers have determined the mechanism that drives chronic organ transplant failure and have identified a potential way to stop the rejection process.
Immunosuppressants are effective at stopping the human body from immediately rejecting transplanted organs. However, while one-year outcomes are excellent, organs start to fail over time and current drugs are ineffective. Attempts to develop new treatments that stop long-term organ failure, known as chronic rejection, have been hindered by questions about why the body starts attacking the transplants.
Writing in Science Immunology, researchers at the University of Pittsburgh describe work to understand the mechanism that causes chronic rejection. The scientists previously identified tissue-resident memory T cells as a key agent in the process. Like all T cells, tissue-resident memory T cells recognize antigens that they have encountered before on threats to the body. The difference is that, while most T cells are found in the blood, tissue-resident memory T cells live in organs.
The new study builds on the earlier work by identifying the factors that maintain resident memory T cells in kidney grafts over time. First author Roger Tieu, PhD, a medical scientist training program student at Pitt, found two factors: the antigens that T cells use to identify transplants as foreign, and the cytokine IL-15.
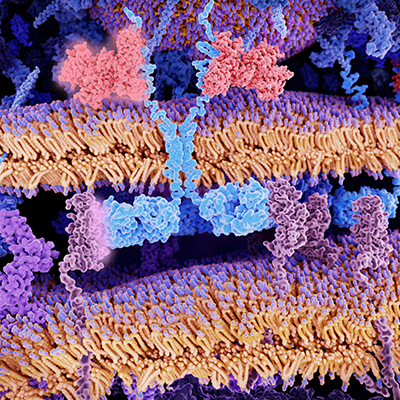
Dendritic cells, another type of immune cell, present the antigen and IL-15 to the memory T cells. By depleting dendritic cells or stopping them from presenting antigen or IL-15, the researchers decreased the number and functionality of tissue-resident memory T cells.
"Antigen and IL-15 are required for T cell maintenance," co-senior author Dr. Martin Oberbarnscheidt, PhD, assistant professor of surgery at Pitt, said in a statement. "If you remove either, resident memory cells decline in number. In a transplant patient, it's not feasible to take the antigen away because it's found throughout the donor organ, but targeting IL-15 is clinically translatable."
Other researchers have studied the effect of blocking IL-15 -- Amgen, for example, ran a phase IIa clinical trial of an anti-Il-15 monoclonal antibody in celiac disease -- and the work suggests that it is possible to safely target the cytokine. In mice, the Pitt researchers found that blocking IL-15 with an antibody prolonged the survival of transplanted kidneys.
Based on the data, the researchers see the potential to study an anti-IL-15 in clinical trials of solid organ transplant patients. In theory, blocking IL-15 could interfere with the organ rejection mechanism without causing the systemic side effects associated with suppression of the broader immune system.
Copyright © 2023 scienceboard.net