March 29, 2023 -- Recent discoveries about how aspirin works to reduce inflammation could lead to alternative medications with fewer side effects. The National Institutes of Health (NIH)-funded research was presented on Tuesday at the annual meeting of the American Society for Biochemistry and Molecular Biology, held March 25-28 in Seattle.
With an estimated 80 billion tablets taken per year, aspirin is one of the most widely used medications in the world. This nonsteroidal anti-inflammatory drug (NSAID) is used to treat pain, fever, and inflammation; an estimated 29 million people in the U.S. also take a low-dose aspirin daily to reduce cardiovascular disease risks. However, even though aspirin has been available commercially since the late 1800s, scientists do not yet fully understand the details of its mechanism of action and cellular targets.
Previous work found that aspirin affixes to the cyclooxygenase, or COX, enzyme, altering its chemical structure and blocking the reaction that produces messenger molecules called prostaglandins, which contribute to pain, inflammation, and fever in response to injury. One prostaglandin, called thromboxane, is produced in blood platelets, causing them to clot and plug up bleeding sites. Even tiny aspirin doses stop thromboxane production, making it useful as a blood thinner.
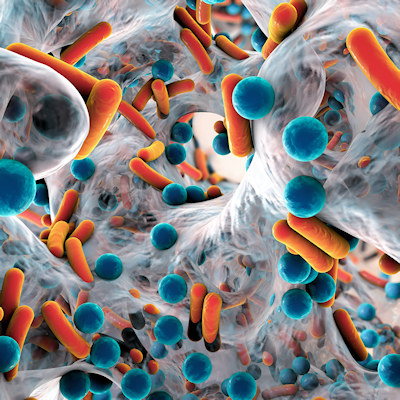
The researchers found that aspirin also controls transcription factors required for cytokine expression during inflammation, while also influencing many other inflammatory proteins and noncoding RNAs that are critically linked to inflammation and immune response.
Metabolism of the amino acid tryptophan plays a central role in the inflammation and immune response. Aspirin slows the breakdown of the essential amino acid tryptophan into its metabolite kynurenine by inhibiting an associated enzyme called indoleamine 2,3-dioxygenase, or IDO1, an enzyme that catalyzes tryptophan oxygenation. This activity significantly suppresses the immune response, mediating inflammation and autoimmune reactions. The researchers found that aspirin downregulates IDO1 expression and its associated kynurenine production during inflammation. Since aspirin is a COX inhibitor, this indicates potential interplay between COX and IDO1 during inflammation.
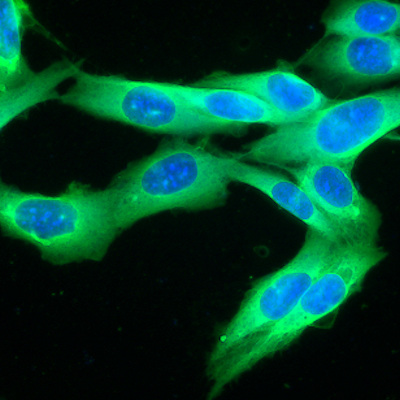
IDO1 is an important target for immunotherapy, a type of cancer treatment that helps the body's immune system seek out and destroy cancer cells. Because COX inhibitors may reverse IDO1-mediated immunosuppression in some cancers, the researchers hypothesize that COX inhibitors might also be useful as drugs to improve immunotherapy responses.
The team is now creating small molecules that modulate COX–IDO1 and plan to explore their potential use as anti-inflammatory drugs and immunotherapeutic agents. The new findings could pave the way to safer aspirin alternatives and improved cancer immunotherapies.
"Aspirin is a magic drug, but long-term use of it can cause detrimental side effects such as internal bleeding and organ damage," Subhrangsu Mandal, co-author and a chemistry professor at the University of Texas, noted in a statement. "It's important that we understand how it works so we can develop safer drugs with fewer side effects."
Copyright © 2023 scienceboard.net