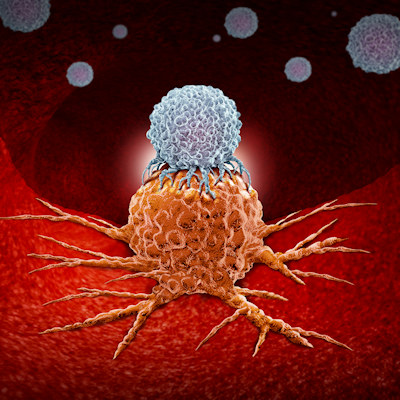
January 3, 2022 -- A new engineered CAR T platform, which turns cells into targeted “micropharmacies” with local activation of small-molecule prodrugs, has been shown to exhibit enhanced antitumor activity and can overcome a variety of current obstacles in conventional CAR T-cell therapy. The research, conducted by Memorial Sloan Kettering (MSK) Cancer Center scientists, was published in Nature Chemical Biology on December 30, 2021.
Conventional CAR T-cell therapies -- genetically engineered versions of a patient’s own immune cells -- are limited to the treatment of B cell cancers and are hindered by several intrinsic factors. Specifically, they are hindered by resistance from antigen-negative tumor cells, meaning they can only kill cancer cells that contain the marker they are designed to recognize. This often leads to issues of “escape” from therapy. Moreover, CAR T cells can become “exhausted” and often are immunosuppressive in the tumor microenvironment.
To improve on the success of current CAR T approaches, a team from MSK Cancer Center’s Sloan Kettering Institute (SKI) explored a novel approach to developing CAR T cells that can generate an orthogonally acting small-molecule drug locally at the disease site. The study's authors note that this is an attractive method for cancer resistance mechanisms.
“Human cells cannot normally make this type of compound,” Derek Tan, PhD, chair of the chemical biology program at SKI, said in a statement. “In contrast to small-molecule drugs, human cells are very good at making enzymes, so CAR T cells are able to produce it effectively.”
The principle behind this approach is logarithmic proliferation triggered by recognition of a target antigen, leading to high concentrations of the therapeutic cells at the disease site, which would in turn enable higher levels of drug amplification. Further, the small-molecule drug at the tumor site would also reduce toxicity associated with systemic administration of the drug.
Developing the new 'armed' CAR T cells
The new CAR T design, termed synthetic enzyme-armed killer cells (Seaker), turns cells into “micropharmacies,” which can deliver a toxic payload directly to a tumor, killing both tumor cells that contain the cancer marker as well as cancer cells nearby that do not. Prodrugs are activated locally at tumor sites, resulting in enhanced anticancer activity in vitro and in vivo, according to the results of the current study.
The Seaker system links a cancer prodrug to another chemical, in this case either glutamate or cephalosporin, that “masks” its function. The genetically engineered CAR T cells are designed to make an enzyme that cuts the masking molecule from the drug. The enzyme acts as scissors, activating the drug at the site of the tumor.
The researchers developed two Seaker systems. The first system is based on Pseudomonas sp. carboxypeptidase G2 (CPG2), which hydrolyzes C-terminal glutamate-masking groups. The second system is based on Enterobacter cloacae β-lactamase (β-Lac), which triggers cleavage of cephalosporin masking groups by hydrolysis of the β lactam.
The systems were examined using a series of stringent in vitro tests to evaluate the activation of several inactive glutamate or cephalosporin-masking prodrugs. Based on potent cytotoxicity and high selectivity indices, the team selected 5′-O-sulfamoyl adenosine (AMS)-Glu and Ceph-AMS for further investigation.
Next, the scientists incorporated the enzymes for the prodrugs into an established CAR T-cell platform to generate Seaker cells CPG2-19BBz and β-Lac-19BBz constructs. They investigated whether the Seaker prodrug combinations could kill antigen-negative cancer cells in vitro in co-culture experiments with both Raji (CD19+) Burkitt’s lymphoma target cells and human factor-independent megakaryoblastic cell line (SET2) leukemia control cells. The combinations were found to have increased efficacy against target antigen-specific tumor cells and antigen-negative cancer cells.
Lastly, mouse models were used to assess if Seaker cells could activate enzymes in vivo and whether Seaker cells could activate the activity of antitumor activity of prodrugs. The team detected active enzymes and consequently decreased tumor bioluminescence when treated with Seaker cells and the corresponding prodrug compared to Seaker cells alone.
“These cells combine the target-seeking power of immune cells with the ability to locally generate a potent anticancer drug for double effect,” said Dr. David Scheinberg, PhD, chair of the molecular pharmacology program at SKI, director of the Center for Experimental Therapeutics at MSK, and lead author of the study.
Platform flexibility provides exciting opportunities
The authors envision the Seaker platform working with several different prodrugs and cleavage enzymes. This could provide an alternative cell therapy solution for a variety of cancers, including solid tumors in which small-molecule drugs could be particularly valuable, as well as other diseases that require local delivery of small-molecule drugs that would otherwise cause dose-limiting toxicities.
“You could imagine it being used to produce drugs to fight other conditions, such as autoimmune diseases and infections,” Scheinberg noted.
A company called CoImmune has licensed the technology from MSK to develop the CAR T-cell technology for human trials. The company expects clinical trials to begin in two to three years.
Do you have a unique perspective on your research related to cell therapy? Contact the editor today to learn more.
Copyright © 2022 scienceboard.net