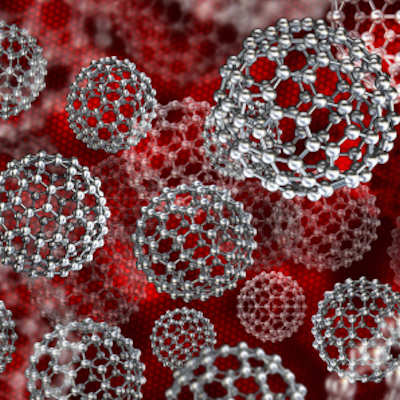
July 22, 2022 -- Researchers at the Massachusetts Institute of Technology (MIT), Broad Institute of MIT, and Harvard University have identified biomarkers that predict whether different types of cancer cells will take up specific nanoparticles, which may help to overcome some obstacles to the development of nanoparticle-based drugs.
Their study, published July 22 in the journal Science, is based on a large-scale analysis of the interactions between 35 types of nanoparticles and almost 500 types of cancer cells, revealing thousands of biological traits that influence whether those cells take up different types of nanoparticles.
The study's authors contend that their findings could enable researchers to better customize drug-delivery nanoparticles to specific cancers by taking advantage of the biological features of certain types of cancer cells.
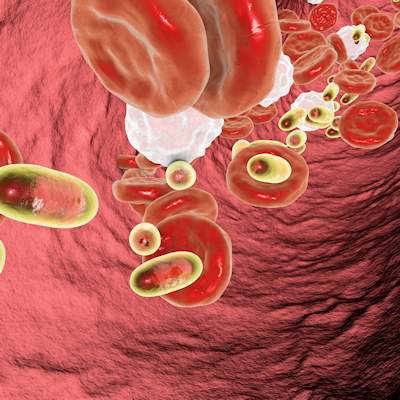
While using nanoparticles to deliver cancer drugs are meant to target tumors with large drug doses while minimizing harmful side effects associated with chemotherapy, to date only a handful of nanoparticle-based cancer drugs have been approved by the U.S. Food and Drug Administration.
As the authors point out, nanoparticle-based treatments can offer various therapeutic advantages such as decreased toxicity, longer half-life, and improved drug delivery. Using their approach, they identified some features of the cancer cells and nanoparticles "that could predict successful nanoparticle delivery" and should facilitate further therapeutic advances.
"We can use this approach to map out what types of nanoparticles are best to target certain cell types, from cancer to immune cells and other kinds of healthy and diseased organ cells. We are learning how surface chemistry and other material properties play a role in targeting," senior author Paula Hammond, PhD, MIT Institute professor, head of the department of chemical engineering, and member of MIT's Koch Institute for Integrative Cancer Research, said in a statement.
The research team adapted the Broad Institute's Profiling Relative Inhibition Simultaneously in Mixtures (PRISM) platform, which was designed to rapidly screen thousands of drugs on hundreds of different cancer types simultaneously, to instead screen cell-nanoparticle interactions. One of the biomarkers researchers identified in their analysis, a protein called SLC46A3, is the subject of further study.
PRISM showed that high levels of the SLC46A3 protein correlated with very low uptake of lipid-based nanoparticles. Researchers subsequently tested these particles in mouse models of melanoma and discovered the same correlation. Their findings suggest this biomarker could be used to assist physicians in identifying patients with tumors likely to respond to nanoparticle-based therapies.
Copyright © 2022 scienceboard.net