June 8, 2020 -- Scientists have identified a new method called ensilication to prevent warmed-up vaccines from degrading. By coating proteins in a silica shell, the structures remain intact and effective. A new study published in Scientific Reports on June 8 expands on previous knowledge about the technique and provides crucial in situ and in vivo evidence for real-world applications.
Biopharmaceuticals such as vaccines and monoclonal antibodies are typically not thermally stable. To increase the shelf-life of these products, they must be stabilized by regulating temperature. However, this can be difficult, as most biopharmaceuticals are vulnerable not only to heating but also to freezing. Fluctuations in temperature can cause aggregation and protein unfolding in biopharmaceuticals, leading to loss of potency.
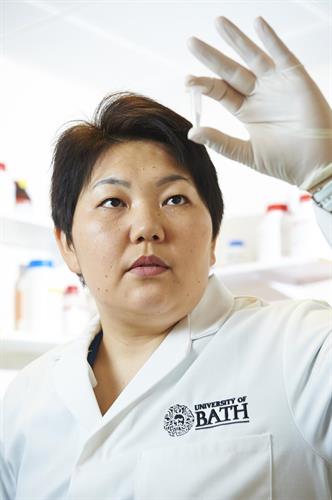
Several approaches have been suggested to increase the thermal stability for storage and transport of vaccines, for example poly-lactic-acid (PLA) or poly-c-glycolic-lactic acid (PGLA), sugar glass, and alginate/chitosan mixtures. A new alternative, called ensilication, was developed two years ago by researchers at the University of Bath in collaboration with the University of Newcastle.
With ensilication, a silica precursor, tetraethyl orthosilicate (TEOS), is hydrolyzed to form orthosilicic acid, which is used to cause rapid polymerization, in which individual proteins can be coated with a form-fitting silica layer. The resulting protein-loaded silica powder is resilient against fluctuations in temperature.
"This is really exciting data because it shows us that ensilication preserves not just the structure of the vaccine proteins but also the function -- the immunogenicity," said Asel Sartbaeva, PhD, lead author from University of Bath Department of Chemistry.
To demonstrate that ensilication can increase thermal stability in lifesaving vaccines, the researchers used the technique to stabilize the tetanus toxin C fragment (TTCF), a component of the full tetanus neurotoxin present in the diphtheria, tetanus, and pertussis (DTP) vaccine. TTCF is a potent immunogen but is susceptible to problems in cold-chain transportation.
At the molecular level, time-resolved small angle x-ray scattering (SAXS) and fitting of mathematical models were used to determine the protein-silica particle formation and characterize the formation of the silica-tailored coating of TTCF. The researchers found that individual TTCF-silica nanoparticles formed and grew over the 10 to 40 seconds of interaction, then began to aggregate into larger clusters. Within minutes, the aggregation of nanoparticles and condensation of silica forms the clusters that make up the dried powdered product.
The researchers performed in vivo experiments with immunized mice either with native or denatured TTCF or ensilicated TTCF. Ensilicated materials were stored for one month at room temperature and transported without specialized equipment.
The researchers found that denatured TTCF did not provide a specific immune response. On the other hand, ensilicated TTCF elicited an immune response that matched native TTCF. This confirms the protective capacity of ensilication to maintain normal protein-epitope conformation at room temperatures.
Silica is an inorganic, nontoxic material that Sartbaeva estimated could be used to extend the shelf-life of vaccines for up to 15 years. She hopes that the silica-wrap protein technique will eventually be adopted to store and transport pediatric vaccines to low-income countries.
"Ultimately, we want to make important medicines stable so they can be more widely available," Sartbaeva explained. "The aim is to eradicate vaccine-preventable diseases in low income countries by using thermally stable vaccines and cutting out dependence on cold chain."
Do you have a unique perspective on your research related to infectious diseases or vaccines? Contact the editor today to learn more.
Copyright © 2020 scienceboard.net