June 4, 2020 -- Using a new genetic engineering technique called base editing, researchers restored genetic hearing loss in mice with a recessive point mutation. The research was published by a group from Boston Children's Hospital, the Broad Institute of the Massachusetts Institute of Technology (MIT), and Harvard University in Science Translational Medicine on June 3.
Hearing loss is one of the most prevalent chronic conditions among children, and several hundred genes have been identified that cause hereditary hearing loss when mutated. There are currently no treatments for any form of hereditary hearing loss.
Scientists have used gene replacement therapies and gene silencing approaches such as antisense oligonucleotides, adeno-associated virus (AAV)-mediated delivery of microRNAs, and genome editing to partially treat hearing loss.
The majority of cases of genetic hearing loss are the result of recessive, loss-of-function point mutations such as c.A545A in the transmembrane channel-like 1 (TMC1) gene that require correction rather than genetic disruption or silencing. Base editing may be a potential one-time treatment strategy to efficiently and permanently correct pathogenic mutations without disrupting the target gene.
"This research is very important for the pediatric community here at Boston Children's Hospital and elsewhere because about 4,000 babies are born each year with genetic hearing loss," said co-senior author Jeffrey Holt, PhD, director of otolaryngology research at the F.M. Kirby Neurobiology Center at Boston Children's Hospital, in a statement. "And, we feel this is a big step beyond the field of hearing restoration and for the broader field focused on treatment of genetic disorders."
To evaluate base editing in a mouse model with recessive hearing loss, the researchers selected Baringo mice, which have recessive, loss-of-function point mutation (c.A545A) in TMC1. TMC1 encodes a protein that forms mechanosensitive ion channels in sensory hair cells of the inner ear and is required for normal auditory function. Mutations in TMC1 account for 4% to 8% of genetic deafness.
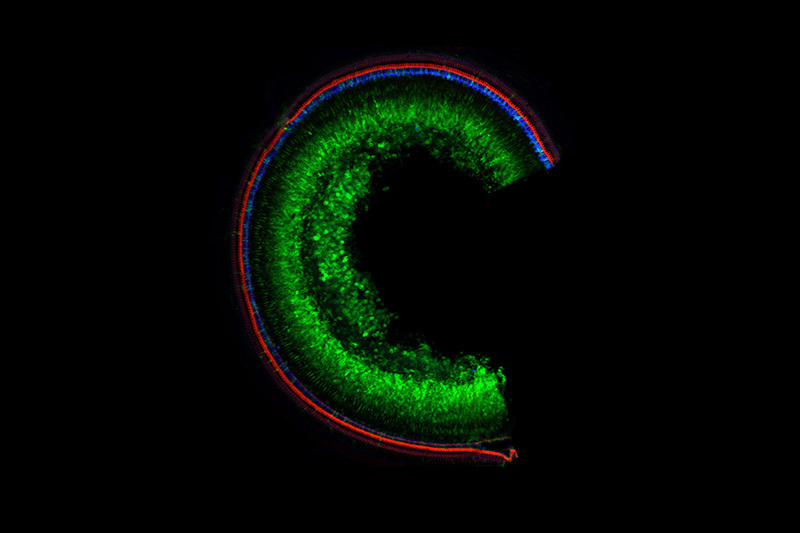
They constructed and evaluated cytosine base editors and three guide RNAs that were packaged into dual AAVs using a split-intein delivery system. The AAVs were injected into the inner ear of mice.
The base editing technique acted like a spell-checker for the TMC1 gene. The researchers reported that the in vivo delivery of the AAVs resulted in 50% base editing efficiency in restoring the wild-type coding sequence of TMC1. Treated mice exhibited normal sensory transduction currents and improved auditory brainstem response thresholds.
If applied in the clinical environment, these improvements in a patient would represent the difference between hearing nothing at all to being able to detect salient auditory cues in the environment, the researchers explained.
Although the data suggest that base editing can repair recessive loss-of-function mutations, the authors also noted that improvements in base editor expression, intein-mediated splicing, and base editing efficiency will be required to further advance the strategy.
"We got it to work but we need to boost the efficiency to make it broadly useful," Holt explained. "But the message is that when we got both [AAVs] into the cells, we went from zero function to 100%. That tells me all we need to do is get it into more cells and we will recover more hearing function."
Over 70 different mutations have been identified in the TMC1 gene in humans.
"We hope this new technique will allow us to pick them off one at a time to restore hearing and balance related to the inner ear," Holt said.
Do you have a unique perspective on your research related to synthetic biology? Contact the editor today to learn more.
Copyright © 2020 scienceboard.net






