May 15, 2020 -- Significantly improved viral clearance and reductions in inflammatory cytokines are observed in COVID-19 patients treated with interferons, according to an exploratory study published in Frontiers in Immunology on May 15.
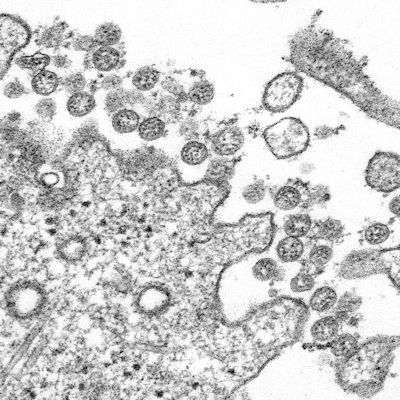
While SARS-CoV-2 continues to spread around the globe without any approved therapies, researchers are urgently searching for effective prophylactic and therapeutic interventions. For instance, type I interferons-alpha/beta (IFNs-α/β) are regulatory proteins that have broad-spectrum antiviral activities that work to directly block viral replication and support immune responses to clear virus infection.
"Interferons are our first line of defense against any and all viruses, but viruses such as coronaviruses have co-evolved to very specifically block an interferon response," explained lead author Eleanor Fish, PhD, of the Toronto General Hospital Research Institute and the University of Toronto Department of Immunology, in a statement. "This informs us of the importance of interferons for the clearance of virus infections. Treatment with interferon will override the inhibitory effects of the virus."
To explore if interferon treatment is a viable therapeutic option for SARS-CoV-2 infection, the researchers treated 77 patients with moderate COVID-19 from Wuhan, China, with IFN-α2b alone or in combination with Arbidol (ARB), a broad-spectrum direct-acting antiviral that induces interferon production and phagocyte activation. The drug displays antiviral activity against respiratory viruses and has been used in past coronavirus outbreaks. The researchers examined viral clearance and circulating cytokine and inflammatory biomarker levels.
In the study, viral clearance was defined as two consecutive negative polymerase chain reaction (PCR) tests. The researchers found that treatment with IFN-α2b, alone or in combination with ARB, accelerated viral clearance by approximately seven days. Reducing the duration of viral shedding could assist in slowing the population spread of the virus.
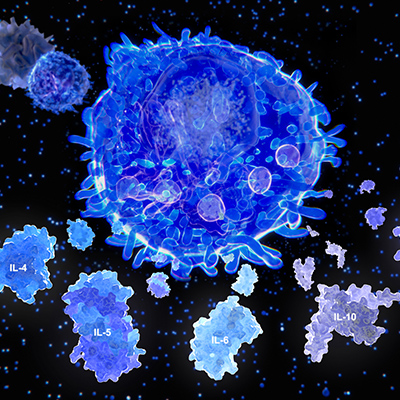
Circulating cytokine levels (interleukin-2 [IL-2], IL-4, IL-10, IFN-gamma [γ], IL-6, tumor necrosis factor-alpha [TNF-α]) and biomarkers of inflammation (C-reactive protein [CRP] and procalcitonin [PCT]) were determined from blood samples over the course of the disease. Generally, most cytokine and biomarker levels remained in a normal range. The two exceptions that the researchers noted were significant decreases in IL-6 and CRP with treatment of IFN. IL-6 has been associated with acute respiratory distress syndrome (ARDS), therefore IFN-α2b has potential as a therapy targeting the cause of the disease (SARS-CoV-2) versus the symptom (blocking IL-6).
Despite the study's small, nonrandomized cohort size, it points to the functional connections between viral infection and host-end organ damage by limiting the subsequent inflammatory response in the lungs of patients.
"Rather than developing a virus-specific antiviral for each new virus outbreak, I would argue that we should consider interferons as the 'first responders' in terms of treatment," said Fish. "Interferons have been approved for clinical use for many years, so the strategy would be to 'repurpose' them for severe acute virus infections. A clinical trial with a larger cohort of infected patients that are randomized to treatment with interferon-alpha or to a placebo would further this research."
Do you have a unique perspective on your research related to immunology or infectious diseases? Contact the editor today to learn more.
Copyright © 2020 scienceboard.net