June 20, 2023 -- Cedars-Sinai Medical Center investigators have identified several steps in the cellular process responsible for triggering one of the body's important inflammatory responses. Their findings, published Friday in Science Immunology, open up possibilities for modulating the kind of inflammation associated with infections and inflammatory diseases.
When the innate immune system -- the defense system humans and other animals were born with -- identifies a potentially harmful bacterium, virus, or other external invader, it unleashes white blood cells to surround and attack the foreign agent. This can cause swelling, redness, heat, and pain in the body's tissues that, in a healthy body, eventually go away. Such inflammation is vital to a functioning immune system and healthy body.
In some people, however, the inflammation phase fails to regress; such prolonged inflammation can wreak havoc on the body. Called chronic inflammation, this condition can damage healthy cells in the body and is associated with serious conditions, including type 2 diabetes, heart disease, and depression. The researchers sought to understand the cellular processes behind inflammation activation, with the goal of finding new treatments to curb chronic inflammation.
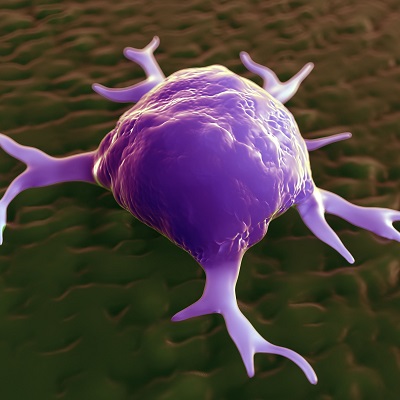
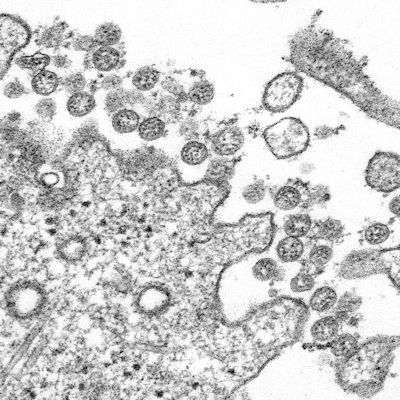
They discovered that an enzyme called hexokinase leaves the mitochondria -- the cell organelle that generates energy -- which jump-starts an immune response. The release of hexokinase destabilizes the mitochondria and alerts the cell that something is wrong. This leads to clustering of the VDAC (voltage-dependent anion channel) protein in the membrane of the mitochondria, which interacts with another protein called NLRP3 (nucleotide-binding domain, leucine-rich–containing family, pyrin domain–containing-3) to initiate inflammasome assembly. The inflammasomes then produce IL-1 beta (interleukin-1-beta), a potent inflammatory protein signal released during many inflammatory responses, and a driver of inflammation.
The investigators studied cells derived from mice to better understand the steps involved in the IL-1 beta pathway. Super-resolution microscopy was used to visualize and measure the steps of this inflammatory process within individual cells. They used inhibitors that block cellular functions as well as gene-editing technology to turn off certain genes and the proteins they express. This allowed them to understand which proteins were vital to triggering inflammation. They believe that being able to target specific steps in this pathway is vital since, in addition to being important for inflammation, the pathway's components also play a vital role in maintaining energy within the cell.
The investigators are continuing to study the cellular steps leading up to, and resulting from, hexokinase's role in the activation of inflammasomes. Since the data points to new drug targets in the inflammatory pathway, they are also using the study results to begin to target this pathway in a variety of inflammatory diseases.
"We now have a clearer understanding of the stepwise process that leads to the production of IL-1 beta," senior and corresponding author Andrea Wolf, assistant professor of biomedical sciences and medicine at Cedars-Sinai, said in a statement. "By understanding the process, we hope to one day find a treatment for diseases associated with this inflammatory response."
Copyright © 2023 scienceboard.net