May 17, 2023 -- A genetic association study comparing participants with Alzheimer’s disease and control participants without Alzheimer’s disease found novel genetic associations between high high-density lipoprotein (HDL) cholesterol concentrations and high systolic blood pressure and a higher risk of Alzheimer’s disease.
These findings, published Wednesday in JAMA Network Open, may inspire new drug targeting and improved prevention strategies.
Dementia is a rapidly increasing health threat worldwide, affecting more than 50 million people and projected to triple in prevalence by 2050. The Lancet Commission for Dementia Prevention, Intervention, and Care's 2020 report estimated that up to 40% of dementia could be prevented or delayed by modifying 12 risk factors throughout life's course. These risk factors are lower education levels, hypertension, hearing impairment, smoking, obesity, depression, physical inactivity, diabetes, low social contact, excessive alcohol consumption, traumatic brain injury, and air pollution.
Culture, poverty, and inequality are key drivers of many of these risk factors. The potential for dementia prevention is especially high in low-income and middle-income countries where more dementia occurs. Individuals who are most deprived will derive the highest benefit, states the report.
However, robust evidence for most of these risk factors is lacking. More-effective interventions appear to target risk factors in the causal pathway to dementia. The researchers working on the recent study sought to comprehensively disentangle potentially causal aspects of modifiable risk factors for Alzheimer's disease to facilitate prevention methods and drug targeting.
This genetic association study included 39,106 participants with clinically diagnosed Alzheimer's disease and 401,577 control participants without Alzheimer's disease. The mean age of the European Alzheimer & Dementia Biobank (EADB)-diagnosed cohort ranged from 72 to 83 years for participants with Alzheimer's disease and 51 to 80 years for control participants. Among participants with Alzheimer's disease, 54% to 75% were female; among control participants, 48% to 60% were female.
The study was conducted using two-sample univariable and multivariable Mendelian randomization. Independent genetic variants associated with modifiable risk factors were selected as instrumental variables from genomic consortia. Outcome data for Alzheimer's disease were obtained from the EADB, generated on August 31, 2021. Main analyses were conducted using the EADB clinically diagnosed end-point data. Analyses were performed between April 12 and October 27, 2022.
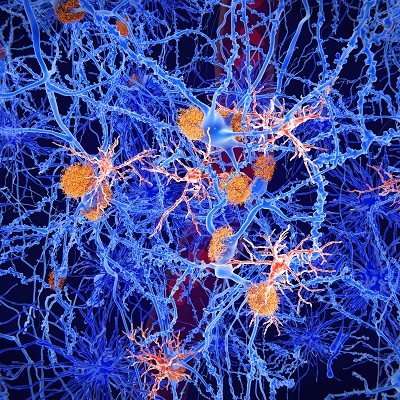
Genetically determined HDL cholesterol concentrations were found to be associated with increased odds of Alzheimer's disease. Genetically determined high systolic blood pressure was associated with increased risk of Alzheimer's disease after adjusting for diastolic blood pressure. In a second analysis to minimize bias due to sample overlap, the entire UK Biobank was excluded from the EADB consortium; after adjusting for diastolic blood pressure, the odds for Alzheimer's disease were found to be similar for HDL cholesterol and systolic blood pressure.
"This genetic association study found novel genetic associations between high HDL cholesterol concentrations and high systolic blood pressure and higher risk of Alzheimer's disease," corresponding author Dr. Ruth Frikke-Schmidt of Copenhagen University Hospital–Rigshospitalet and her colleagues concluded in the paper. "These findings may inspire new drug targeting and improved prevention implementation."
Copyright © 2023 scienceboard.net