January 5, 2023 -- UNC Lineberger Comprehensive Cancer Center researchers have found that measuring immune system B-cell activation may be better at predicting HER2-positive breast cancer's response to treatment than measuring either T-cell activation or the total number of immune cells around a tumor. The study, published January 5 in the journal JAMA Oncology, may allow doctors to be more precise in choosing which drugs and which regimen to use in treating this form of the disease.
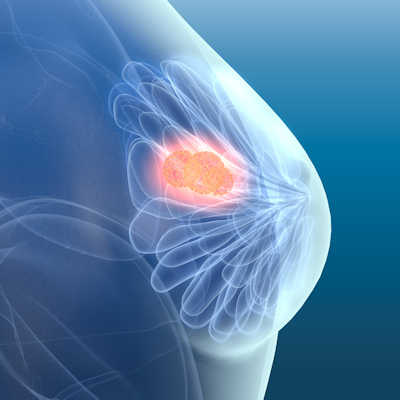
In HER2-positive breast cancer, the human epidermal growth factor receptor 2 (HER2) protein is overexpressed on breast cell surfaces. This breast cancer is often treated with trastuzumab, a drug that targets the HER2 protein. However, the immune system plays a key role in patient responses to such drugs.
Important immune cells include B cells, which create antibodies that neutralize cancer cells and infections, and T cells, which directly fight cancers and infections. When there are many active immune cells circulating around a tumor, called tumor-infiltrating lymphocytes (TILs), the cancer tends to be easier to treat and cure. Hence, determining immune cell activity could allow doctors to identify which HER2-positive breast cancer patients might do well with standard, or even minimized, therapy.
The researchers combined the results of two large clinical trials focused on HER2-positive breast cancer, called CALGB 40601 and PAMELA. The 305 patients enrolled in CALGB 40601 received trastuzumab, paclitaxel (a standard chemotherapy drug), lapatinib (an inhibitor that blocks HER2 action), or a combination of these drugs, for 16 weeks. The 151 patients in PAMELA received trastuzumab and lapatinib for 18 weeks. All patients subsequently underwent tumor-removal surgery.
While TILs were associated with breast cancer elimination in both trials, six of seven B-cell immune signatures were most strongly associated with higher elimination rates. The six B-cell signatures were also associated with better survival rates, while TILs were not.
Since different breast cancers have molecularly distinct features with differing biological bases and outcomes, better biomarker tools are needed to guide treatment escalation and de-escalation -- particularly for difficult-to-treat HER2-positive and triple-negative breast cancers. The researchers hypothesize that a similar analysis in triple-negative breast cancer might show similar results. Their large, integrated database combines gene expression and clinical data, including response to therapy and survival outcomes from over 1,000 women participating in clinical trials.
"The analysis of these data will provide essential information for biomarker development and precision medicine in HER2-positive breast cancer and the insights will inform clinicians when someone may need more -- or less -- chemotherapy, and more -- or less -- anti-HER2 drugs," said first author Dr. Aranzazu Fernandez-Martinez, PhD, a UNC oncologist, in a statement.
Copyright © 2023 scienceboard.net