October 6, 2020 -- Specialized nanoparticles can be used to deliver small interfering RNA (siRNA) to the bone marrow where they can turn off specific genes in bone-marrow endothelial cells to help treat heart disease or boost stem cell production, according to new research published in Nature Biomedical Research on October 5.
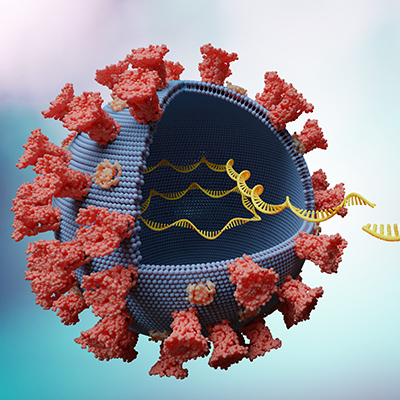
Human bone marrow is the source of thousands of hematopoietic stem cells and progenitors that release billions of blood cells into circulation every day. RNA interference (RNAi) therapeutics, a type of genetic therapy, can influence protein expression within hematopoietic environments and as such can be used to silence nearly any gene within the body. However, a challenge for many RNAi therapeutics is its delivery to appropriate tissues. When injected into the bloodstream, nanoparticles carrying RNA tend to accumulate in the liver.
"If we can get these particles to hit other organs of interest, there could be a broader range of disease applications to explore, and one that we were really interested in in this paper was the bone marrow," explained lead author Michael Mitchell, PhD, former Massachusetts Institute of Technology (MIT) postdoc and assistant professor of bioengineering at the University of Pennsylvania, in a statement. "The bone marrow is a site for hematopoiesis of blood cells, and these give rise to a whole lineage of cells that contribute to various types of diseases."
Nanoparticles to deliver RNA
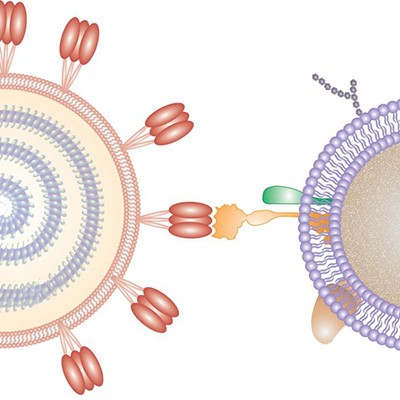
Nanoparticle delivery systems can be used to deliver RNA to organs other than the liver. The research group, led by Robert Langer, PhD, David H. Koch Institute professor at MIT, has previously described a nanoparticle formulation coated with lipids that can silence genes in the lung.
"RNA nanoparticles are currently FDA-approved as a liver-targeted therapy but hold promise for many diseases, ranging from COVID-19 vaccines to drugs that can permanently repair disease genes," said senior author Daniel Anderson, PhD, professor of chemical engineering at MIT. "We believe that engineering nanoparticles to deliver RNA to different types of cells and organs in the body is key to reaching the broadest potential of genetic therapy."
In the current study, the researchers developed a RNAi approach that is capable of delivering siRNA to endothelial cells in the bone marrow.
They started by screening a library of nanoparticles based on a class of nanoparticle-forming materials that were generated by combinatorial chemical synthesis and ability to deliver siRNA to lung endothelium in vivo. The researchers enhanced nanoparticle siRNA delivery by modulating the nanoparticle polyethylene glycol (PEG) architecture of 15 variants. One of these, NicheEC-15, was able to escape entrapment in the liver and lungs. They confirmed that NicheEC-15 had higher uptake into bone-marrow endothelial cells and could successfully silence targeted genes in vivo.
siRNA two ways
Next, the team conducted a series of proof-of-concept experiments, where they silenced endothelial cell expression of two quintessential hematopoietic niche factors. The first, stromal-derived factor 1 (Sdf1), is a molecule that normally prevents hematopoietic stem cells from leaving the bone marrow. Turning off this gene could improve stem cell yield in stem cell transplantation.
The researchers found that the RNAi approach decreased Sdf1 expression by two-fold and increased the release of progenitor cells from the bone marrow by five-fold. In vivo, the researchers demonstrated that the isolated stem cells as a result of the RNAi therapy could differentiate into new blood cells when transplanted into another mouse.
"We are very excited about the latest results," said Langer. "Previously we have developed high-throughput synthesis and screening approaches to target the liver and blood vessel cells, and now in this study, the bone marrow. We hope this will lead to new treatments for diseases of the bone marrow like multiple myeloma and other illnesses."
The second target, monocyte chemotactic protein 1 (Mcp1), has the opposite effect, triggering release from the bone marrow. Mcp1 protein is released by bone-marrow cells after a heart attack. It stimulates a flood of immune cells to leave the bone marrow and travel to the heart, where the protein promotes inflammation and can lead to further heart damage. Silencing this gene can be helpful in the treatment of chronic inflammatory conditions such as cardiovascular disease.
The RNAi approach in silencing Mcp1 was able to dampen leukocyte traffic and reduce inflammation. In mice, the researchers found that that delivering RNA that targets Mcp1 reduced the number of immune cells that went to the heart after a heart attack. Mice that received this treatment also showed improved healing of heart tissue following a heart attack.
"We now know that immune cells play such a key role in the progression of heart attack and heart failure," said Mitchell. "If we could develop therapeutic strategies to stop immune cells that originate from bone marrow from getting into the heart, it could be a new means of treating heart attack. This is one of the first demonstrations of a nucleic-acid-based approach of doing this."
Do you have a unique perspective on your research related to genetics or cell biology? Contact the editor today to learn more.
Copyright © 2020 scienceboard.net