January 13, 2023 -- Baylor College of Medicine and Washington University School of Medicine researchers studied posoleucel, an investigational off-the-shelf T-cell therapy that simultaneously targets six different viruses. The results, published January 11 in the journal Clinical Cancer Research, showed promising antiviral efficacy and safety in a phase II clinical trial of patients who had undergone stem cell transplantation to treat blood diseases including cancer.
Patients with blood cancers may be treated with allogeneic stem cell transplantation (allo-SCT), a procedure in which the patient's stem cells are replaced with donor stem cells. However, those patients are highly susceptible to viral infections that can be fatal. The antiviral medications currently available often have limited efficacy and difficult-to-tolerate toxicities for these patients. Improved treatment options are needed, including the ability to target multiple viruses with a single therapy.
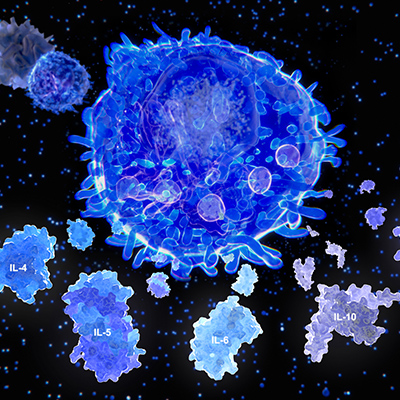
Posoleucel, an allogeneic therapy comprising donor T cells, targets six of the most common viruses in patients following allo-SCT: adenovirus, BK virus, cytomegalovirus (CMV), Epstein-Barr virus, human herpes virus 6, and JC virus. Posoleucel is the first T-cell therapy to target BK virus, which can cause severe, painful bladder infections requiring immediate treatment. Since posoleucel utilizes healthy donor T cells rather than T cells from the patient or transplant donor, it avoids an otherwise lengthy development process, making it more readily available.
The trial enrolled 58 adult and pediatric patients who had undergone allo-SCT to treat blood diseases and had at least one of the six viral infections targeted by posoleucel. There were 70 total viral infections in the trial population, primarily from CMV and BK virus. Eligible patients were unresponsive to or unable to tolerate standard therapies. Responses were defined as complete -- a viral load reduction to normal range with complete symptom resolution, or partial -- a 50% minimum viral load reduction or 50% symptom improvement.
Of the 58 patients, 55 (95%) responded to posoleucel within six weeks of infusion. The circulating virus amount was reduced by an average of 97% in these patients. Among the 12 patients with more than one viral infection, 10 (83%) responded. Within six weeks of treatment, 83% of the 12 adenovirus patients responded, as did 100% of the 27 BK virus patients, 96% of the 24 CMV patients, 100% of the two Epstein-Barr virus patients, and 75% of the four human herpes virus 6 patients. The one JC virus patient showed initial stabilization, but eventually died.
No patient experienced cytokine release syndrome, an acute systemic inflammatory condition. Thirteen patients (22%) reported acute graft-versus-host disease (GvHD); however, only four were considered new cases. Most skin flares, the most common GvHD symptom, were successfully treated. Randomized phase III clinical trials evaluating posoleucel are currently underway.
"An exciting observation from this study was that posoleucel could be administered within 24 hours in some cases, with symptom resolution in a matter of days in some patients," noted Texas Children's Hospital pediatric hematologist-oncologist and senior author Dr. Bilal Omer in a statement.
Copyright © 2023 scienceboard.net