October 29, 2021 -- Researchers have identified a diagnostic signature for genetic mutations and other abnormalities associated with drug resistance and poor outcomes in estrogen receptor positive (ER+) metastatic breast cancers. The findings, published on October 28 in Cancer Research, may one day guide personalized treatments for cancer patients.
The MOTERA gene signature, which stands for mutant or translocated estrogen receptor alpha, can accurately predict the presence of dangerous chimeric fusion proteins, which are created through the joining of two or more genes that may code for different proteins, or ligand binding domain mutations on the protein coding gene ESR1.
The work was done at the laboratory of Dr. Matthew Ellis, PhD, professor and director of the Lester and Sue Smith Breast Center at Baylor University in Texas.
Mutant estrogen receptors
About 70% of breast cancers are initially diagnosed as estrogen receptor alpha positive (ERα+), which means they have receptors for estrogen and receive signals from the estrogen hormone 17-β estradiol for growth. Treatments usually induce endocrine deprivation; for example, by targeting the ERα ligand binding domain through hormonal drug therapies such as tamoxifen or fulvestrant. However, cancer cells may become resistant to drugs or evade treatment.
"One of the predominant ways ER+ breast cancer cells evade treatment is by creating mutant ERs that no longer can be recognized and targeted by ER-targeting cancer drugs," first author Xuxu Gou, a graduate student in the Ellis lab, said in a statement.
The research team had been studying mutations and translocations on ESR1, a protein coding gene on the sixth chromosome associated with breast cancer. In a translocation, a segment from one chromosome is transferred to and reattaches to a different chromosome.
ER-related translocations create chimeric ER proteins, meaning the protein contains only half of the ER protein, with the other half coming from a different protein. Some of these chimeras are harmless, but many can be harmful, such as, for example, when the drug-binding region of the protein is replaced, rendering the breast cancer cells immune to ER-targeting drugs.
"Not all ER translocations were active -- some drive metastasis and resistance to treatment, but others do not," Gou said. "To be able to determine whether any particular ESR1 translocation can promote disease progression, we developed a diagnostic genetic signature that detects the presence of an active ESR1 chimeric protein."
The team functionally screened 15 chimeric ESR1 fusions, of which 10 were identified as "active" fusions that promoted cancer cell growth, motility, invasion, epithelial-mesenchymal transition, and resistance to the drug fulvestrant.
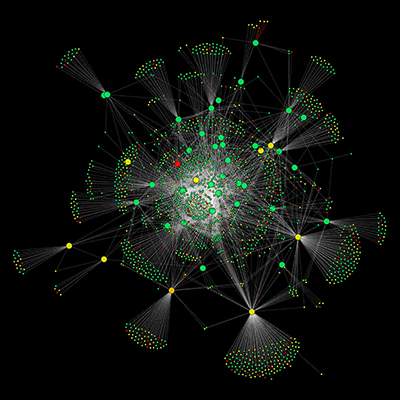
24-gene signature identified
Using RNA sequencing, the team then identified a gene expression pattern specific to these functionally active ESR1 gene fusions that they subsequently reduced to a diagnostic 24-gene signature.
Next, they identified the 24-gene signature in a dataset created from genomic and transcriptomic analysis of 20 mice xenografted with ER+ patient-derived tumors that demonstrated different degrees of dependence on estrogen for growth. Surprisingly, the same 24-gene signature also turned out to be associated with common ligand binding domain point mutations in ESR1 that are also associated with drug resistance and poor outcomes.
Finally, these findings from the mouse models were replicated in data from 55 human patients in a human metastatic breast cancer cohort. The fact that a single diagnostic gene signature can identify both point mutations and translocations associated with poor outcomes makes it efficient from a diagnostic perspective, according to the authors.
"The 24-gene signature represents an efficient approach to screening samples for the presence of diverse somatic ESR1 mutations and translocations that drive endocrine treatment failure in MBC [metabolic breast cancer]," they wrote.
The scientists believe that once their diagnostic approach becomes more fine-tuned, specific treatment approaches for tumors expressing these characteristics can be developed.
"In the future, a patient's cancer cells could be analyzed and, once the MOTERA score indicates the presence of an ER mutation or translocation, then the tumor cells would be further studied to more precisely determine what kind of ER mutant or translocation is present," co-author Charles Foulds, PhD, assistant professor at the Lester and Sue Smith Breast Center, said. "This would help guide the selection of a personalized, optimal treatment."
Do you have a unique perspective on your research related to transcriptomics or genomics? Contact the editor today to learn more.
Copyright © 2021 scienceboard.net