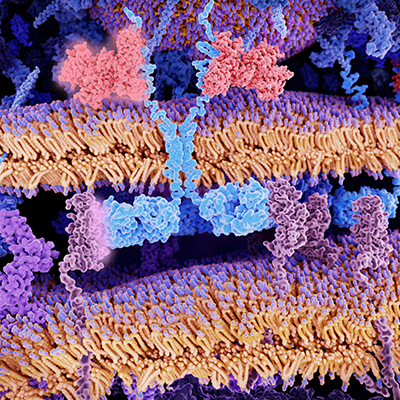
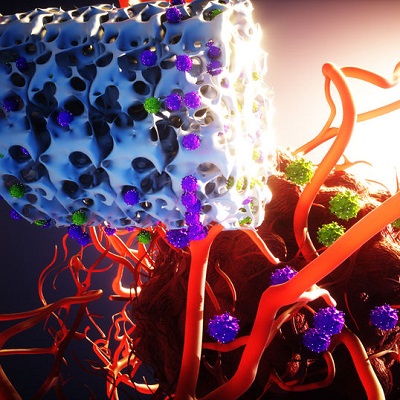
August 4, 2022 -- A Boston Children’s Hospital lab has developed a new method that could make chimeric antigen receptor (CAR) T-cell therapy more widely available using induced pluripotent stem cells (iPSCs) to develop mature immune cells.
The proprietary differentiation process is designed to overcome the tendency of iPSCs to generate immature, embryonic blood cell types by suppressing the enzyme EZH1 and giving the iPSCs the ability to make mature T cells.
The technique, developed by the lab of Dr. George Daley, PhD, in the Boston Children's Hospital Stem Cell Program, is described in a study published August 4 in Cell Stem Cell.
According to the paper, iPSC T cells derived in a stroma-free, serum-free system following repression of EZH1 (referred to as EZ-T cells) showed a molecular signature more closely resembling mature TCRαβ T cells found in adult blood.
"We show that generic iPS cells can be converted to CAR T cells not only more efficiently, but more effectively -- creating an enhanced CAR T cell that more faithfully resembles the gold-standard clinical-grade cells we currently use," Daley, senior author of the paper, said in a statement. "Our strategy could enable 'off-the-shelf' CAR-T therapies and help more patients access these treatments."
Boston Children's Hospital and ElevateBio, a cell and gene therapy development company in Waltham, Mass., are forming a new company (not yet named) around the technology, according to the announcement. In a separate press release, ElevateBio announced the formation of the company with Daley and the hospital to develop allogeneic iPSC-derived immunotherapies.
ElevateBio CEO David Hallal in a statement said the new company is the first to emerge from the previously announced five-year cell and gene therapy collaboration between Boston Children's Hospital and ElevateBio.
Copyright © 2022 scienceboard.net