August 31, 2020 -- A wide variety of symptoms and organs are involved in SARS-CoV-2 infection. This phenomenon could be explained by the distribution of the virus's gateway receptor, which is found in tissues throughout the body. Characterization of angiotensin-converting enzyme 2 (ACE2) expression is detailed in a recent Cellular and Molecular Neurobiology article.
During severe COVID-19 disease, systemic infection hyperimmune responses can lead to cytokine storm and multiorgan failure in about 3% of cases. COVID-19 is also associated with several neurological symptoms including loss of smell, altered taste, loss of coordination, and headache and nausea, among others.
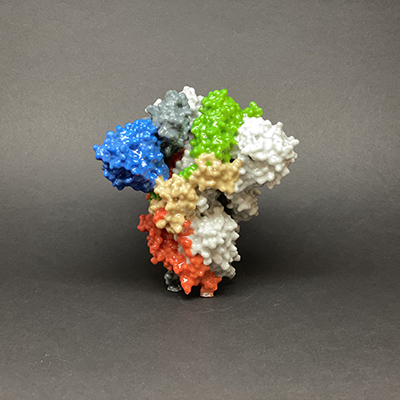
SARS-CoV-2 gains entry into the body through the ACE2 gateway receptor. This single-pass type I transmembrane receptor is exposed on multiple cell types, including type II alveolar cells of the respiratory system, enterocytes and intestinal epithelial cells, endothelial cells, epithelial cells of the eye, kidney cells, certain immune cells (alveolar monocytes and macrophages), and central nervous system cells of the cerebral cortex and brainstem.
Exclusive binding of SARS-CoV-2 to ACE2 results in endocytosis and translocation of the virus into endosomes. These specific molecular mechanisms are currently under intense research investigation as a way to identify and develop therapeutic strategies.
Because of the widespread distribution of ACE2 in the body and its critical importance in the recognition, attachment, and entry of SARS-CoV-2 into cells, researchers from Louisiana State University (LSU) investigated the expression of ACE2 in 85 human tissues and 21 regions of the brain. They used human multiple tissue expression arrays to quantify tissue-specific ACE2 messenger RNA (mRNA) expression.
The researchers found that ACE2 was ubiquitously expressed throughout most tissues of the body. The highest expression was found in the vascular, gastrointestinal tract, respiratory, excretory, and reproductive tissues.
The enzyme may play a significant role in the regulation of functions in the respiratory, cardiovascular, gastrointestinal, and renal-excretory system. SARS-CoV-2 may take advantage of the widespread receptor to gain cellular entry and promote its survival and proliferation in multiple cell types.
Furthermore, variable ACE2 receptor expression has been tied to age, sex, ethnicity, medication, and several comorbidities (cardiovascular disease, metabolic syndrome, obesity, and dementia) that could potentially indicate susceptibility to SARS-CoV-2 infection or the severity of COVID-19 disease.
"Besides strong ACE2 expression in respiratory, digestive, renal-excretory and reproductive cells, high ACE2 expression was also found in the amygdala, cerebral cortex, and brainstem," said Walter Lukiw, PhD, professor of neuroscience, neurology, and ophthalmology at LSU Health New Orleans Neuroscience Center of Excellence and School of Medicine. "This may help explain cognitive deficits associated with SARS-CoV-2 infection. Some of the highest ACE2 expression levels were found in the pons and medulla oblongata in the human brainstem, an anatomical region of the brain containing the medullary respiratory centers, and this may in part explain the susceptibility of many [COVID-19] patients to severe respiratory distress."
The researchers also found high ACE2 expression in the eyes, suggesting that the eyes may be vital entry points for SARS-CoV-2 invasion. Therefore, they propose that eyeglasses or face shields might help reduce SARS-CoV-2 transmission.
"Several important research gaps remain," Lukiw concluded. "A real danger of SARS-CoV-2 infection is not only its highly transmissible and contagious nature and lethality, but also its simultaneous and multipronged attack on many human cell and tissue types involving vital and critical respiratory, immunological, vascular, renal-excretory and neural systems as well as an unprecedented coordinated disruption of the complex neurophysiology, neurochemistry, neurobiology and neurology of the cells of the brain and central nervous system that normally regulate these multiple physiological systems."
Do you have a unique perspective on your research related to infectious diseases or neuroscience? Contact the editor today to learn more.
Copyright © 2020 scienceboard.net