May 13, 2020 -- An overreaction of the immune system to SARS-CoV-2 -- a phenomenon known as cytokine storm -- has emerged as a major contributor to patient mortality during the COVID-19 outbreak. In a recent series of papers, authors examined cytokine storm and offered perspectives on preventing it from occurring.
In the first article, a review published in Frontiers in Public Health, experts from Zunyi Medical University in China summarized the epidemiology, disease pathway, symptoms, diagnosis, and current treatment of severe COVID-19. They explained how the virus infects the airways and causes cytokine storm, an overactivation of white blood cells that leads to severe cases of the COVID-19 respiratory disease.
In a second article, published in Cancer and Metastasis Reviews, U.S. researchers postulated that controlling local and systemic inflammatory response in COVID-19 may be as important for treatment as antiviral therapies. They discussed how blocking specific mediators of the immune response to SARS-CoV-2 could work to treat the disease.
Insights into cytokine storms
The full extent of pathogenesis of COVID-19 is still unclear. However, several factors have been confirmed to be involved in the progression of the disease.
Specifically, SARS-CoV-2 binds to angiotensin-converting enzyme 2 (ACE2) receptors through the coronavirus spike protein to invade alveolar epithelial cells to promote direct toxicity and excessive immune responses. The systemic inflammation causes a cytokine storm, resulting in lung injury. Because ACE2 is expressed in the kidneys, heart, lung, and intestines, SARS-CoV-2 can invade cells in these tissues to proliferate and destroy organs.
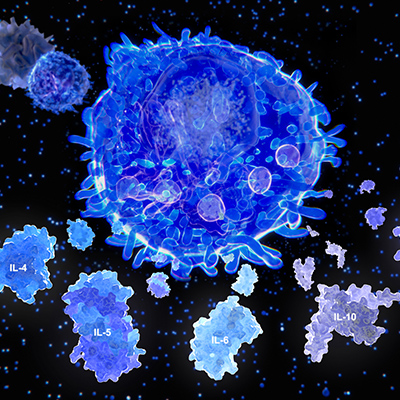
The authors of both publications suggested that excessive proinflammatory responses are a hallmark of severe COVID-19 cases. Cytokine storms, the overproduction of cytokines by white blood cells in response to the virus, can quickly lead to systemic organ failure.
The Zunyi researchers explained that the poor outcomes of COVID-19 patients are associated with significantly elevated levels of interleukin-2 (IL-2), IL-6, IL-7, IL-10, granulocyte colony-stimulating factor (GCSF), interferon gamma-induced protein 10 (CXCL10), monocyte chemoattractant protein-1 (MCP-1), macrophage inflammatory protein-1 alpha (MIP-1α), and tumor necrosis factor-alpha (TNF-α). Furthermore, excessive activation of lymphocytes in COVID-19 patients leads to an increase of proinflammatory CCR4+CCR6+Th17 cells. These helper T cells secrete cytokines and cause further immune-mediated damage.
The U.S. researchers agreed that cytokine storms involving the release of proinflammatory cytokines (TNF-α, IL-6, IL-1, IL-8, and MCP-1) may lead to rapid systemic organ failure observed in severe COVID-19 patients. However, the authors suggested that SARS-CoV-2 also causes massive cell death and cellular debris due to the activation of inflammasomes that trigger a macrophage-derived "eicosanoid storm," a surge of proinflammatory bioactive lipid mediators that fuels local inflammation.
Potential therapies to treat proinflammatory responses
The authors of the Front Public Health review article suggested that in the absence of a specific antiviral cure for COVID-19, the goal for treatment must be to fight symptoms through intensive maintenance of organ function; for example, an artificial liver blood purification system or renal replacement therapy to filtrate the blood through mechanical means. They noted that it is especially important to supplement or replace lung function by a variety of ventilation measures.
"Because treatment for now relies on aggressive treatment of symptoms, preventative protection against secondary infections, such as bacteria and fungi, is particularly important to support organ function, especially in the heart, kidneys, and liver, to try and avoid further deterioration of their condition," explained author Daishun Liu, PhD, from Zunyi, in a statement.
Alternatively, the U.S. researchers suggested that the deployment of anti-inflammatory agents can lead to the resolution of inflammatory responses by clearing cellular debris. These specialized proresolving mediators (SPMs) include resolvins, lipoxins, and protectins and work against the release of proinflammatory cytokines and chemokines. SPMs promote antiviral B lymphocytic activity in influenza, suggesting that they may be a promising therapy for COVID-19.
Another promising therapeutic intervention may be soluble epoxide hydrolase (sEH) inhibitors, which prevent lung inflammation and improve lung function. They downregulate the transcription regulator of NF-κB, the center of eicosanoid storms, and promote the resolution of proinflammatory pathways.
"What is exciting for us is that these lipid mediators that 'turn off,' or resolve, inflammation are already in clinical trials for other inflammation-driven diseases, such as eye disease, periodontal disease, and pain," said author Dr. Dipak Panigrahy, an assistant professor of pathology at Beth Israel Deaconess Medical Center, in a statement. "The mediators can quickly be applied to turn off inflammation in COVID-19 patients."
Do you have a unique perspective on your research related to immunology or infectious diseases? Contact the editor today to learn more.
Copyright © 2020 scienceboard.net