June 29, 2021 -- Researchers have developed a new framework to uncover pathophysiological and molecular features that determine the effectiveness of immunotherapies. The research, published in Nature Communications on June 29, provides an opportunity for improving patient care and gaining a deeper understanding of cancer immunotherapy mechanisms.
Immunotherapies such as adjuvant checkpoint inhibitors and combination immunotherapies, including antiprogrammed cell death 1 (anti-PD-1) and anticytotoxic T-lymphocyte-associated protein 4 (anti-CTLA-4), have demonstrated significant patient survival benefits in melanoma patients. By comparison, the treatment of glioblastoma multiform with immunotherapies has not been effective to date.
The administration of a neoadjuvant (presurgical) checkpoint blockade should result in certain pathophysiological and molecular features in the tumor. But the exact nature (similarities and differences) of those features across tumor types and from patient to patient have yet to be characterized.
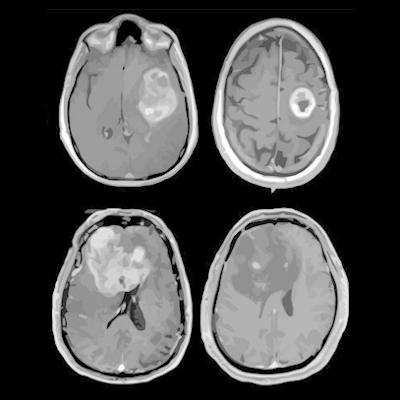
To elucidate some of the underlying cellular changes caused by cancer immunotherapies, a team of scientists led by researchers from the Institute for Systems Biology conducted a comparative analysis of tumor tissues collected from patients with recurrent glioblastoma or high-risk melanoma and treated with a neoadjuvant immune checkpoint blockade.
They examined tumor tissues collected from 13 patients with recurrent glioblastoma and 23 patients with high-risk melanoma, with both sets of patients treated with neoadjuvant immune checkpoint blockade therapy.
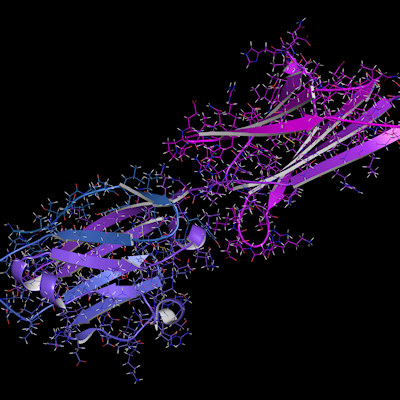
Then they developed a framework utilizing multiplex spatial protein profiling, machine learning-based image analysis, and data-driven computational models to investigate the pathophysiological and molecular factors within the tumor microenvironment that influence treatment responses. The team sought to make three distinct sets of comparisons:
- Compare the levels of a protein panel collected from microscopic compartments within both classes of tumors
- Determine the correlates of cytotoxic CD8+ T cells and treatment responses in both tumors with a computational approach called micro-tumor analysis
- Map out the immune cells in both tumors and compare their degree of immune cell–cell interaction using a method called immune neighbor analysis
The researchers used the melanoma tumor analyses as a guide for the interpretation of the glioblastoma tissues.
"This work reveals similarities shared between glioblastoma and melanoma, immunosuppressive factors that are unique to the glioblastoma microenvironment, and potential cotargets for enhancing the efficacy of neoadjuvant immune checkpoint blockade," said Yue Lu, PhD, a co-author and postdoctoral fellow at the Institutes for Systems Biology, in a statement.
The team found that melanoma tumors, especially those that respond to immunotherapy treatment, exhibit extensive immune-cell rich areas, while immune-cell rich regions within glioblastoma tumors were sparse and contained just a few cells. Another key difference was that higher immune cell–cell interaction was predictive of therapy response in melanoma but not in glioblastoma.
For glioblastomas, there are no single proteins that can be measured that would give an indication that immunotherapy treatment was effective. The presence of CD8 and major histocompatibility complex class I antigens predict therapy responses in melanomas but not glioblastomas. By identifying the proteins within immune-rich regions, the researchers found that the glioblastoma molecular response to immunotherapy depends on signatures of tumor aggressiveness and on the presence of neutrophils and myeloid cells.
"This framework can be used to uncover pathophysiological and molecular features that determine the effectiveness of immunotherapies," added Alphonsus Ng, PhD, co-author and postdoctoral fellow at the Institutes for Systems Biology.
The authors noted that the techniques developed in the current study should enable increased levels of quantitation, including cell-type specificity for various protein markers for other types of cancers.
"We believe that the integrated biological, clinical and methodological insights derived from comparing two classes of tumors widely seen as at the opposite ends of the spectrum with respect to immunotherapy treatments should be of interest to broad scientific and clinical audiences," said Jim Heath, PhD, corresponding author and president and professor at the Institutes for Systems Biology.
Do you have a unique perspective on your research related to cancer research? Contact the editor today to learn more.
Copyright © 2021 scienceboard.net