November 16, 2022 -- While more than 100 clinical trials targeting the checkpoint protein T-cell immunoreceptor with Ig and ITIM domains (TIGIT) are now underway, two large phase III trials recently failed to improve cancer outcomes. However, a new analysis of the immunosuppressive KIR2DL5/PVR pathway provides a potential explanation for why anti-TIGIT therapies have failed in the clinic.
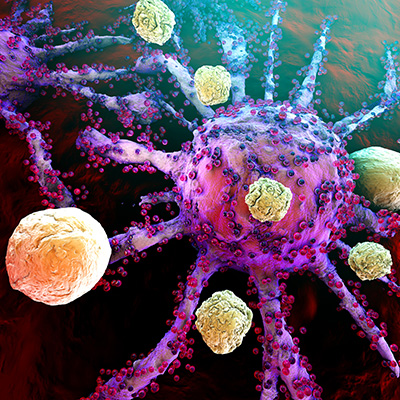
Evidence that the cancer-cell protein PVR inhibits the activity of T cells and natural killer (NK) cells by binding to TIGIT has attracted the attention of multiple biopharma companies in recent years but data from the first phase III studies have disappointed, with the failure of Roche's prospect in two lung cancer tests prompting others to reconsider their own strategies.
Now, scientists at Albert Einstein College of Medicine have published a paper that may offer insights into why anti-TIGIT antibodies have so far failed to live up to the expectations of drug developers that have bet hundreds of millions of dollars on the molecules.
In a paper published November 15 in the Journal of Clinical Investigation, the researchers describe an analysis of KIR2DL5 -- a receptor that, like TIGIT, binds to PVR. Noncompetitive binding of KIR2DL5 and TIGIT to PVR suggested that both receptors function simultaneously and independently. Also, blockade of the TIGIT/PVR axis left the KIR2DL5/PVR pathway intact, offering a mechanistic explanation for the recent clinical setbacks.
"TIGIT blockade had a minimal effect on NK cell cytotoxicity, whereas KIR2DL5 blockade markedly restored the cytolytic activity of NK cells. Thus, the existence of KIR2DL5-mediated inhibition of NK cells in the [tumor microenvironment] represents a substantial obstacle to the success of the blockade of TIGIT. Indeed, we observed KIR2DL5+ immune cells infiltrated in various human cancers that highly expressed PVR," the researchers wrote.
KIR2DL5 suppressed NK cell cytotoxicity against multiple solid and blood tumor cells in a PVR-dependent manner. Blockade of KIR2DL5 with a monoclonal antibody enhanced NK-mediated anticancer immunity in vitro and inhibited tumor growth and improved mouse survival across multiple humanized mouse models. KIR2DL5's binding site on PVR is distinct from that of TIGIT.
The findings suggest that the PVR protein may suppress the activity of NK cells by binding to KIR2DL5, not TIGIT. To explore that theory, the researchers have developed a monoclonal antibody that targets the KIR2DL5/PVR pathway and are interested in partnering to advance and commercialize the technology.
"We believe the novel immunotherapy we've developed has great potential to move into clinical trials involving various types of cancer," study leader Xingxing Zang, PhD, a professor at Einstein, said in a statement.
Copyright © 2022 scienceboard.net