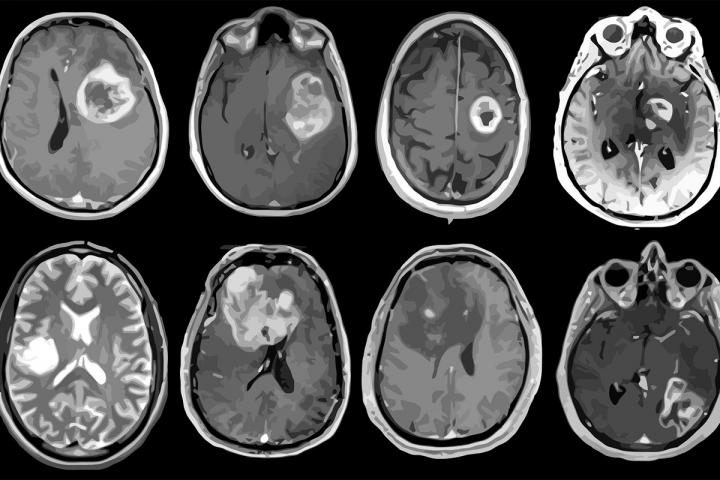
February 11, 2021 -- A team of more than 40 investigators has created a profile of the genes, proteins, infiltrating cells, and signaling pathways of the deadly brain cancer glioblastoma. The findings could lead to better patient care, according to the authors of a new study published February 11 in Cancer Cell.
The study illuminates the biology of glioblastoma, wrote a group led by senior author Li Ding, PhD, of Washington University in St. Louis, MO. The research was a collaboration established by the National Cancer Institute of the U.S. National Institutes of Health in Bethesda, MD.
Promising immunotherapies have emerged for the treatment of glioblastomas, including immune checkpoint inhibitors, vaccines, chimeric antigen receptor (CAR) T-cell therapy, and viral therapy. Yet none of these options have been successfully cleared for clinical use, likely due to varying responses among patients.
"To improve therapies for this deadly cancer, understanding the tumor cells themselves is important but not enough," Ding said in a statement released by Washington University. "We also must understand the tumor cells' interactions with the surrounding environment, including immune cells and the connective tissues and blood vessels."
Although rare, glioblastoma is the most aggressive of cancers, and it has high mortality rates, with fewer than 10% of patients surviving longer than five years after a diagnosis, Ding's group noted. Unfortunately, research on the genomic features of glioblastoma has not led to more successful treatment.
In the current study, the authors integrated proteogenomic and metabolomic data from 10 platforms. Some of the platforms included whole genome sequencing (WGS), RNA sequencing (RNA-seq), and mass spectrometry analysis of the phosphoproteome. These tools were used to investigate 99 treatment naive glioblastomas prospectively, measuring proteins in the samples as well as protein modifications called phosphorylation and acetylation, which influence how cells communicate.
Multiomics analysis revealed a subset of patients who exhibit shortened overall survival. The phosphoproteomic data indicated that two proteins, protein tyrosine phosphatase nonreceptor type 11 (PTPN11) and phospholipase c, gamma 1 (PLCG1), are a signaling hub for multiple receptor tyrosine kinases that drive tumor growth. RNA and protein expression data indicate that glioblastoma subtypes also differ in infiltrating macrophages and distribution of specific immune cell types. Furthermore, the study revealed an association between histone (H2B) acetylation and patterns of protein expression associated with immune cell functions in glioblastoma.
"Acetylation changes a protein's shape and often results in opening up DNA-protein complexes to facilitate gene expression. By adding protein acetylation to our study, we were able to complete the loop from proteins to genes and gene expression, shedding light on important regulatory changes in glioblastoma," said co-senior author Karin Rodland, PhD, chief scientist for biomedical research at Pacific Northwest National Laboratory.
The research also suggested that glioblastoma tumors may respond differently to different treatments based on their unique "immune landscape," the investigators noted. They identified four categories of this landscape that are made up of varying combinations of T cells and immune cells called macrophages; immunotherapies that targets macrophages may work well in patients with high numbers of these cells but not as well in patients with lower numbers. Clinical trials that lump all patient types together may miss when a drug is actually working.
"These patterns provide additional information for researchers to understand how the glioblastoma subtypes they identified may vary in biological function," said co-author Tao Liu, PhD, of Pacific Northwest National Laboratory in Richland, WA, in the statement.
The research could lead to better clinical trial design that could translate into more tailored treatment for patients, according to co-author Dr. Milan Chheda of Washington University.
"For most clinical trials, we take all comers and give them the same treatment," he said in the university statement. "We are not designing trials in the most precise way because we have not fully understood the molecular differences between each patient's tumor. This leads us to call a treatment a failure when in fact it may be helping specific people."
Copyright © 2021 scienceboard.net


