July 28, 2021 -- A protein that controls calcium signaling within heart cells could help prevent chronic heart failure, according to the results of a new study published in Nature Communications on July 28. The findings point to the protein as a therapeutic target for drugs that could alleviate heart failure.
Chronic heart failure is a growing global epidemic. Dilated cardiomyopathy -- one of the most common causes of heart failure -- is a condition where the ventricular chambers of the heart are enlarged with impaired blood-pumping ability, potentially associated with alterations in the function of contractile proteins and excitation-contraction coupling. This condition can be caused by abnormalities in calcium homeostasis, resulting in contractile dysfunction and, ultimately, heart failure. Thus, calcium plays a crucial role in these functions.
In between heartbeats, calcium levels in heart cells are low and enable the heart to relax. Subsequently, a large amount of calcium is released from the sarcoplasmic reticulum, which facilitates cellular contraction. The ebb and flow of calcium levels in heart muscle cells keeps the heart beating.
Mitochondria, the powerhouse of the cell, also play a role during this process and rely on calcium to produce biochemical energy that keeps cells alive. However, the exact mechanisms of calcium signaling in the mitochondria -- and the connection to cardiovascular health -- are not well understood.
Calcium flux into the mitochondrial matrix primarily occurs through the inner membrane via the mitochondrial calcium uniporter. However, knockout mouse models lacking the mitochondrial calcium uniporter do not show any adverse cardiac phenotype. This suggests another protein plays a role in calcium dynamics within the heart.
Voltage-dependent anion channel 2 (VDAC2) is an outer mitochondrial membrane protein that plays an important role in calcium signaling. Initial calcium import into the intermembrane space of the mitochondria occurs through VDACs. It is also known that the interaction between the mitochondrial outer membrane and the sarcoplasmic reticulum is crucial for mitochondrial calcium signaling.
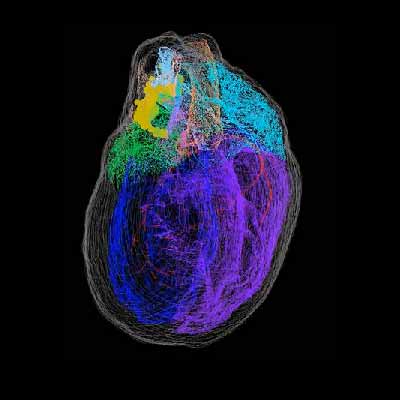
Therefore, researchers from University of Utah Health hypothesized that mitochondrial calcium dynamics are impacted by VDAC2 and play a critical role in cardiac function. To test the hypothesis, the team generated a cardiac ventricular myocyte-specific developmental deletion of VDAC2 in mice.
In the study, loss of VDAC2 in the myocardium caused severe impairment in excitation-contraction coupling by altering both intracellular and mitochondrial calcium signaling. This led to cardiac remodeling, which progressed to severe cardiomyopathy and death.
Specifically, differential gene expression and western blot data suggest that loss of VDAC2 leads to abnormalities in cellular calcium signaling pathways. In myocytes (heart cells), VDAC2 knockout caused a significant disruption in calcium signaling, which may contribute to declines in myocardial function.
Immunoprecipitation assays also revealed crosstalk of VDAC2 with two sarcoplasmic reticulum proteins: ATPase sarcoplasmic/endoplasmic reticulum Ca2+ transporting 2 and sodium-calcium exchanger 1. Disruption of these interactions causes changes in calcium signaling in heart cells.
"Based on our human and laboratory research, it appears that if VDAC2 is not working properly, then everything in the heart can cascade downward from there," said senior author Stavros Drakos, PhD, professor of medicine and director of cardiovascular research for the division of cardiology at University of Utah Health, in a statement. "If we can figure out ways to help this protein do its job again, then it's possible that we might be able to address heart failure far earlier in the disease process."
To this end, the team reintroduced VDAC2 in 6-week-old knockout mice using an adeno-associated virus 9 vector and found that the treatment partially rescued the disease phenotype.
Cumulatively, the data suggest that VDAC2 is crucial for cellular calcium cycling and normal cardiac function, thereby making it a plausible therapeutic target for heart failure. The researchers found that activation of VDAC2 by the antiarrhythmic drug efsevin (a synthetic dihydropyrrole carboxylic ester compound) increased cardiac contractile force in a mouse model of pressure overload-induced heart failure.
"Our study shows the importance of VDAC2 in normal cardiac function," noted lead author Thirupura Sundari Shankar, a doctoral candidate in Drakos' lab. "Through this unique role, VDAC2 emerges as a potential therapeutic target for heart failure patients."
Do you have a unique perspective on your research related to drug discovery and development? Contact the editor today to learn more.
Copyright © 2021 scienceboard.net