August 18, 2020 -- Rare stem cells that give rise to neutrophils in human bone marrow could offer a path to developing treatments for diseases that involve the white blood cells, according to a new article published in Immunity on August 18.
Neutrophils are white blood cells that are an essential component of the innate immune system. They have a short lifespan in the blood and are constantly replenished from progenitors in the bone marrow. Therefore, neutrophils are attractive targets for cancer immunotherapies since they exist in a high density within some tumor microenvironments.
Neutrophil differentiation is a complex, multistep process that begins with granulocyte-monocyte progenitors that are developed from common-myeloid progenitors. Researchers over the last decade have worked to refine the classification of these progenitors and their ability to generate downstream subsets.
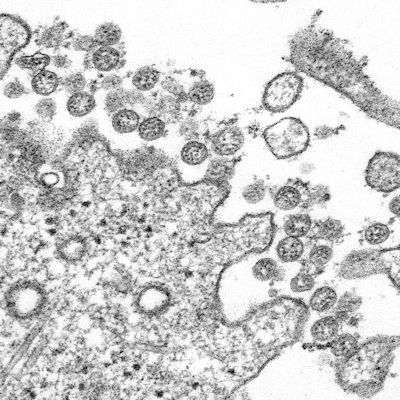
Scientists from the La Jolla Institute for Immunology have recently identified human neutrophil progenitors (hNePs) and confirmed their status as neutrophil progenitors. Another research group has described a proliferative bone marrow neutrophil (preNeu) population that differentiates into nonproliferating immature and mature neutrophils. The relationship between these two types of cells is unclear and the researchers aimed to clarify the relationship using mass cytometry.
"We have identified the stem cells that are the early origins of neutrophils, the most abundant blood cell type in humans," said Huy Dinh, PhD, a former La Jolla Institute for Immunology postdoctoral associate who recently moved to a faculty position at the University of Wisconsin-Madison, in a statement. "Knowing how human neutrophils develop is especially relevant today because immature neutrophils have been found to be elevated in both the blood and lungs of severe COVID-19 patients."
The researchers used mass cytometry and cytometry by time-of-flight (CyTOE) to distinguish the rare neutrophil progenitor cells from other types of immune progenitor cells. They identified five neutrophil subsets (N1-N5) in human bone marrow by profiling 35 surface protein markers (cytokine receptors).
N1 expressed a marker associated with neutrophil precursors CD49d and lacked maturation markers including CD11b, CD16, CD101, and CD10. The defining marker of subset N1 was CD71, a protein involved in iron metabolism. This group contains neutrophils at the very earliest stages of neutrophil development compared to the other four groups. The N1 subset showed similar surface marker expression to preNeus.
A different group of progenitor cells, hNePs, were previously thought to contain a homogenous population of CD66b+CCD117+ neutrophils. However, the research revealed that hNePs contain a heterogeneous population of both CD71+ and CD71-, with the CD71- population containing markers of mature neutrophil subsets. The CD71+ hNePs were termed "early neutrophil progenitors" (eNePs).
The preNeu-like subset contained a rare CD71+CD117+ population of eNePs. These are the earliest neutrophil progenitors identified. The researchers concluded that eNePs preceded preNeus in neutrophil development.
The research also made it possible to identify more specific protein markers on the early progenitor cell surface. So, while CD117 expression is not specific for progenitor populations, in combination with CD66b and CD71, it reliably identifies human neutrophil progenitors.
RNAseq was used to understand the molecular characteristics of the different neutrophil subsets. The team found that eNePs are developmentally early neutrophils sharing similarities with the N1 subset, compared to other subsets with the highest expression of neutrophil progenitor genes and lower expression of genes specific to mature neutrophils. Here again, the researchers found evidence that eNePs are likely upstream progenitors of the preNeu subset.
Abnormal expression of chemokines and cytokines during many types of cancer are associated with an increase in neutrophils and neutrophil precursors. Therefore, high concentrations of immature neutrophils in the bloodstream can be a tell-tale sign of cancer and even a biomarker for COVID-19.
Neutrophil development has been in the news recently due to the COVID-19 pandemic, as studies have shown immature neutrophils are also more abundant in some patients with COVID-19.
"We need to study this phenomenon further to see if these neutrophils can be tied to case prognosis or if they can be a drug target for COVID-19," Dinh explained.
Do you have a unique perspective on your research related to immunology? Contact the editor today to learn more.
Copyright © 2020 scienceboard.net