July 20, 2021 -- Cellular reprogramming of ex vivo cells may offer improvements on first-generation adoptive cell therapies, which have experienced limited clinical success due to complex manufacturing, potential patient rejection, and availability of clinical cell types. Further, in vivo reprogramming may expand on this concept by eliminating the need for manufacture and the risk of immune rejection.
The clinical success of anti-CD19 CAR T-cell therapies has not only provided efficacious treatment alternatives for cancer patients but also aided the developmental and regulatory precedent for the translation of cell-based therapies for other disease areas. The first-in-class nature of these adoptive products means their success is likely to be constrained by the novelty of the approach, influencing manufacturing complexity and the cost of delivery.
Furthermore, the ability to isolate and expand cells of sufficient therapeutic quality and quantity in a patient-to-patient model can limit progress. To date, over 10 advanced cell therapy products have been approved -- the majority of which are T-cell-based and strictly autologous.
Developing next-generation cell therapies centers around the enhancement of efficacy, safety, and accessibility. While considerable emphasis is being placed on modalities and modifications for overcoming rejection, developers must also focus on exhaustion, affinity, and mitigating the risk of adverse events.
Techniques such as cellular reprogramming will allow the exploration of scalable allogeneic cell sources and the optimizable generation of cells for therapeutic development.
Cellular reprogramming
Cellular reprogramming involves remodeling gene expression to generate a desired cell lineage or type. This concept gained prominence following Shinya Yamanaka's discovery of induced pluripotent stem cells (iPSCs) in 2007. Over a decade later, there has been considerable focus on the generation of iPSC-derived cell types for therapeutic application; though, their potential remains limited due to the need to recapitulate complex biological pathways through lengthy and complex differentiation protocols.
Advances in single-cell technologies and exponential growth of high-resolution biological data, harnessed by high-throughput bioinformatics and computational methodologies, have enabled the introduction of systematic means for controlling cellular identity. Such technologies sidestep the trial-and-error approach employed by Yamanaka. They leverage transcriptomic and epigenetic data to systematically identify key regulatory switches, such as the optimal combination of transcription factors or growth factors, required to directly differentiate any source cell type to any target cell type, as well as maintain cell identity. This circumvents the need for any intermediary steps and reduces the time required to produce a cell type for therapeutic use.
Transforming ex vivo cell therapy
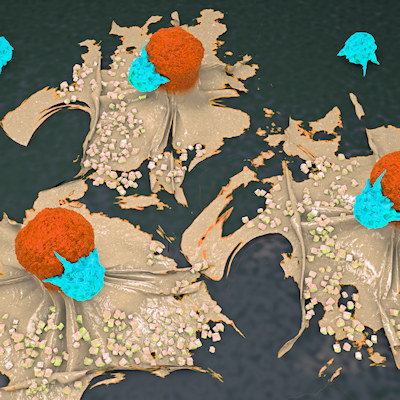
Prior to the invention of CAR, cell therapies were largely limited to allogeneic hematological transfusion and transplantation. Coupled with well-established in vitro culture and expansion protocols for T lymphocytes, CAR enabled the antigen-directed cytotoxicity of T cells to be harnessed, expanding the scope of cell therapy.
First-generation ex vivo cell therapies, such as autologous anti-CD19 CAR T cells, demonstrated the clinical value and curative potential of enhancing the therapeutic qualities of immune and other patient-derived cell types. Optimizing these first-in-class approaches focuses on improving their safety and efficacy profile via a plethora of modifications, including targeting tumor-associated antigens, incorporating control switches, and employing gene editing to prevent graft-versus-host disease and/or other toxicity risk components.
These adaptations improve efficacy and limit the risk of adverse events but do little to address the aforementioned roadblocks associated with ad-hoc manufacture and commercial viability of autologous approaches. As a result, developmental trends have shifted toward an allogeneic approach, seeking to replace autologous cell sources with consistent and scalable alternatives, such as iPSCs.
The benefits of an allogeneic "off-the-shelf" cell therapy approach are clear: batch-producing cells derived from an unrelated donor or universal cell source that can be used to treat many patients. However, this brings with it a comparable set of challenges in acquiring therapeutic cell types: producing quality cells that exhibit functional maturity and developing robust and current good manufacturing practice (cGMP)-compliant production processes.
Computational approaches to cellular reprogramming are uniquely positioned to address these challenges, through several methods:
- First, through systematized directed differentiation or transdifferentiation, it is possible to produce any clinically valuable or even difficult-to-obtain cell types or subtypes from any starting cell type, such as iPSCs.
- Second, such approaches provide the ability to replicate the in vivo microenvironment, enabling the maintenance and expansion of those cells in vitro, while also promoting functional maturity.
- Finally, by combining these approaches to optimize the production and maintenance of cells, it is likely to enhance the efficiency and standardization of the manufacturing processes and subsequently the development of scalable, cost-efficient ex vivo cell therapies.
Pioneering in vivo reprogramming therapy
The shift from autologous to allogeneic therapy is a crucial step in addressing scalability and patient access to cell-based therapies; however, ex vivo manufacturing challenges remain, particularly when considering the process variability between cell type, indication, or disease area. To this point, cell transdifferentiation has the potential to lead to new therapeutic modalities, such as the reprogramming of cells in vivo to forego ex vivo manufacture.

In vivo reprogramming is made possible through the delivery of a combination of regulatory factors via a delivery vector directly to the disease site, tissue, or organ in need of functional restoration. With the support of the in situ microenvironment, these regulatory factors induce the expression of cell identity genes to drive the conversion and maintenance of functionally mature cells directly in the human body.
To date, proof-of-concept studies have demonstrated the feasibility of in vivo reprogramming as an approach for a number of diseases, including animal studies demonstrating superior functional maturity of induced cardiomyocytes in vivo, overall improvement in cardiac function, and reduced fibrosis. In the pancreas, in vivo reprogramming is being explored for the generation of insulin-secreting pancreatic beta cells and as an alternative to allogeneic beta-cell transplants requiring concomitant immunosuppressive therapy. The reprogramming of neurons, especially from astrocytes prevalent throughout the central nervous system, has drawn significant interest in in vivo development.
Further evaluation of the safety and efficacy of such approaches will be required; however, advancements in single-cell sequencing and the subsequent development of computational methods, applicable to the conversion of cells in situ, will expedite the development of systematic and reproducible in vivo reprogramming approaches.
In preclinical development, direct cellular reprogramming technologies such as Mogrify are being leveraged to develop in vivo reprogramming therapies for unmet medical needs in ophthalmology. Visual impairment is most often the result of an inherited genetic trait or degeneration.
Treatment is available but limited to gene therapy against mutations in RPE65 and autologous retinal pigment epithelium transplantation for retinal degeneration. In cases where the underlying mechanisms are more complex, either involving various mutations or multiple cell types, there is currently no treatment available. Introducing an optimal combination of regulatory factors in vivo to affect an in situ conversion of ocular cell types could help treat retinal degeneration.
The future of cell therapies
The incorporation of data-driven cell reprogramming technologies into the cell therapy development life cycle, accompanied by the exponential growth of omics data and profiling of therapeutic cell types, enhances and accelerates the development of ex vivo cell therapies, including those generated from an "off-the-shelf" iPSC-derived source. Extending this method to apply direct cellular conversion capabilities in vivo could enable a new class of reprogramming therapies, leveraging the regenerative potential of cells and tissues within our bodies to address diseases with unmet clinical needs in a direct and efficacious manner.
Rodrigo Santos, PhD, is the director of cell technologies at Mogrify.
Do you have a unique perspective on your research related to cell therapy or immunology? Contact the editor today to learn more.
Copyright © 2021 scienceboard.net