September 17, 2020 -- A new study stressed the importance of a multilayered, virus-specific immune response for controlling SARS-CoV-2 during acute COVID-19, with an emphasis on the critical nature of T cells over antibodies during the process. The work was published in Cell on September 16.
Since SARS-CoV-2 appeared, researchers have been trying to understand why the immune system sometimes does more harm than good during infection. When SARS-CoV-2 infiltrates the body, the innate immune system elicits a broad and unspecific attack against the intruders. The waves of signaling molecules that result in inflammation alert the adaptive immune system to mount a precise attack against the pathogen, which is when the viral particles are intercepted, and infected cells are eliminated.
The adaptive immune system responds to pathogens in an antigen-specific way to develop protective immunity. It consists of three major lymphocyte types:
- B cells that produce antibodies
- CD4+ T cells (helper T cells)
- CD8+ T cells (cytotoxic T cells and killer T cells)
Assessments of antigen-specific T cells and neutralizing antibodies in acute COVID-19 are still lacking, according to researchers at La Jolla Institute for Immunology.
To assess the three arms of antigen-specific adaptive immune response to SARS-CoV-2 and to correlate immune responses to COVID-19 disease severity, researchers collected blood samples from 50 COVID-19 patients and analyzed all three branches of the adaptive immune system. The cohort included cases across a range of COVID-19 disease severities.
"It was particularly important to us to capture the whole range of disease manifestation from mild to critically ill so we could identify differentiating immunological factors," explained co-first author and infectious disease specialist Dr. Sydney Ramirez, PhD, who spearheaded the sample collection.
The researchers found that broad and coordinated adaptive immune responses among the three branches of the adaptive immune system were associated with lesser COVID-19 disease severity. They suggest that CD4+ and CD8+ T cells are key for control and clearance of acute infection and can help elicit high-quality neutralizing antibodies.
"When we looked at a combination of all of our data across all 111 measured parameters we found that in general, people who mounted a broader and well-coordinated adaptive response tended to do better," said co-first author and postdoctoral researcher Carolyn Moderbacher, PhD. "A strong SARS-CoV-2 specific T cell response, in particular, was predictive of milder disease. Individuals whose immune response was less coordinated tended to have poorer outcomes."
Interestingly, the researchers did not find evidence of adaptive immune cells being causally involved in COVID-19 pathogenesis (i.e. cytokine storm). In the cohort, hospitalized patients had similar CD8+ T-cell response cytokine profiles as nonhospitalized patients, and TH2 and TH17 cytokines from CD4+ T cell responses were normal. In fact, the team observed quite the opposite effect where strong SARS-CoV-2 specific CD4+ and CD8+ T-cell responses were associated with low disease severity.
Aging and adaptive immune responses in COVID-19
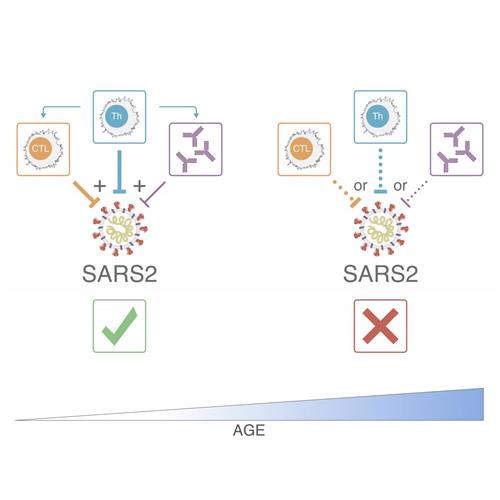
In the study, low abundance of naïve T cells was also associated with severe COVID-19 disease in the cohort. Naïve T cells are inexperienced T cells that have not yet been differentiated. As individuals age, the reservoir of naïve T cells dwindles, and as fewer cells are available for activation, it can become increasingly difficult to respond to new pathogens.
"This could either lead to a delayed adaptive immune response that is unable to control a virus until it is too late to limit disease severity or the magnitude of the response is insufficient," Moderbacher explained.
"People over the age of 65 were much more likely to have poor T cell responses, and a poorly coordinated immune response, and thus have much more severe or fatal COVID-19," said senior author Shane Crotty, PhD, professor at the La Jolla Institute Center for Infectious Disease and Vaccine Research. "Thus, part of the massive susceptibility of the elderly to COVID-19 appears to be a weak adaptive immune response, which may be because of fewer naïve T cells in the elderly. With increasing age, the reservoir of T cells that can be activated against a specific virus declines and the body's immune response becomes less coordinated, which looks to be one factor making older people drastically more susceptible to severe or fatal COVID-19."
Vaccines and adaptive immune responses
Most human vaccines work on the basis of protective antibody responses, with neutralizing antibodies being the most common mechanism of action. Vaccine antibodies provide protective immunity when present prior to exposure to a pathogen. Once the virus appears, vaccine-induced antibodies are ready to intercept it.
Therefore, many COVID-19 vaccines under development focus on producing strong neutralizing antibody responses. However, nearly all antibody responses and affinity-matured B cell memory depend on CD4+ T cells and are therefore essential for vaccines.
Separately, studies have shown that CD8+ T cells are important in the development of protective immunity against viral infections. The results of the study also indicate that while neutralizing antibodies play a role in resolving acute COVID-19, they appear to be less important than SARS-CoV-2 CD4+ or C8+ T cells.
"Thus, these findings indicate it is plausible T cells are more important in natural SARS-CoV-2 infection, and antibodies more important in a COVID-19 vaccine, although it is also plausible that T cell responses against this virus are important in both cases," Crotty said.
Do you have a unique perspective on your research related to immunology? Contact the editor today to learn more.
Copyright © 2020 scienceboard.net