June 21, 2021 -- A new accessible and scalable protocol for manufacturing in vitro lung cell models could have applications in the development of new therapies for respiratory viral infections and drug toxicology studies on human lungs. Details about the protocol were published in Stem Cells on June 21.
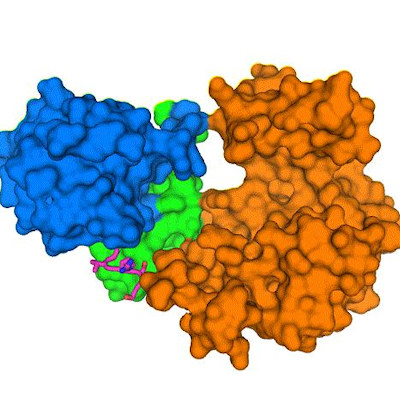
COVID-19 has demonstrated that there is an urgent need for in vitro systems that can assess the effect of infectious or foreign agents in the lungs. SARS-CoV-2 predominately infects airway and alveolar epithelial cells using the angiotensin-converting enzyme 2 (ACE2) receptor for entry.
In vitro models mimicking the human airways can be a useful tool for assessing toxicology, drug discovery, and viral infection studies. Despite the numerous advantages of these systems, their availability is limited to primary samples, which can differ significantly based on the donor's genetic background.
Stem cell-based in vitro models
Using induced pluripotent stem cells (iPSCs) can overcome the limitations of primary cells. These cells can be reprogrammed to become every other cell type in the body, including those making up the airways. Additionally, iPSCs can propagate indefinitely to provide a large supply of cells with the genetic background of a single donor, rather than the varied backgrounds of the multiple donors hindering primary pulmonary epithelial cell models.
To this end, a team led by Newcastle University researchers developed a protocol to generate airway epithelial basal-like cells from iPSCs to simplify the manufacturing process for cellular models of human airways.
In the study, basal-like cells were cultured on transwell inserts to allow formation of a confluent monolayer and then exposed to an air-liquid interface to induce differentiation into a pseudostratified epithelial construct with a marked similarity to human upper lung cells in vivo.
Importantly, the scientists demonstrated that the cells produced mucus and functional cilia and could support SARS-CoV-2 infection and replication and the secretion of cytokines in a manner similar to that of humans. Using immunofluorescence and flow cytometry, the team found that the model cells express genes associated with a basal cell phenotype (KRT14, deltaNp63, NGFR, Integrin alpha 6) while maintaining their multipotent capacity.
The unique combination of the monolayer differentiation protocol and transfer of the 3T3 (mouse embryonic fibroblasts)/Rho kinase inhibitor (to limit cell death and dedifferentiation) system at an early stage of development (differentiation day 14) provided an effective protocol for enriching airway basal-like cells, the authors noted.
Testing the model
The researchers tested the newly developed model by infecting iPSC-derived constructs with SARS-CoV-2. The team confirmed the presence of surface proteins (ACE2 and transmembrane protease, serine 2) to which the virus could attach, and which are necessary for cell invasion. They found that viral replication occurred with the release of virions at the apical surface of the constructs, as confirmed by plaque-forming unit assays and immunofluorescence analyses. In parallel to SARS-CoV-2 infection, the scientists quantified the number of viral particles and secretion of cytokines and chemokines produced.
The model provides an approximation of how the human airway epithelium works, which could be useful for studying respiratory infectious diseases and toxicology of foreign substances in the lungs, according to the authors. Moreover, the model is helpful because it is able to produce a substantial number of cell types, which can be efficiently recovered from cryopreservation, making it a cost-effective method to produce large numbers of airway constructs.
"The infected model cells also secreted cytokines at levels corresponding to the behavior of the airway epithelium in the body following SARS-CoV-2 infection," said corresponding author Lyle Armstrong, PhD, professor of stem cell sciences at Newcastle University, in a statement. "Our protocol not only simplifies the manufacture of cellular models of the human upper airways, but it has a distinct advantage in that we have eliminated the need for primary samples that differ in genetic backgrounds. Our next step will be to expand on this model by including immune cell components."
Do you have a unique perspective on your research related to infectious diseases or virology? Contact the editor today to learn more.
Copyright © 2021 scienceboard.net