May 1, 2019 -- In 2018, the International Agency for Research on Cancer reported more than 18 million people were diagnosed with cancer. Between 40 and 45 million people worldwide are living with cancer and nearly 9.6 million people die. Cancer deaths occur in about 50% of people who develop cancer in developed countries; this is in contrast to 80% death rate in cancer patients in underdeveloped countries. The numbers are staggering. But there is hope, as scientists around the globe work on developing new technologies, in the form of targeted therapies, to combat the incidence of cancer.
Currently, cancer treatment often includes a combination of therapies; surgery, chemotherapy, hormone therapy or targeted therapy. The problem with many of the 'broad' or traditional therapies is that they damage healthy cells while trying to eliminate cancerous cells. Targeted therapies are among the most promising scientific developments in cancer treatment.
WHAT ARE TARGETED THERAPIES?
Targeted therapy is defined as the use of specific treatments and drugs tailored to each patient and to various types of cancer, in order to stop the spread of cancerous cells in the body with as few side effects or damage to healthy cells as possible. Advances in this field are coming fast and furious, according to specialists, and many new therapies work on a molecular level, using biological agents to stop cancerous and abnormal cells in their tracks.
According to the National Cancer Institute (NIH), targeted cancer therapies are different from standard therapies in the following ways:
- Targeted therapies act on specific molecular targets that are associated with cancer, whereas most standard chemotherapies act on all rapidly dividing normal and cancerous cells.
- Targeted therapies are deliberately chosen or designed to interact with their target, whereas many standard chemotherapies were identified because they kill cells.
- Targeted therapies are often cytostatic (that is, they block tumor cell proliferation), whereas standard chemotherapy agents are cytotoxic (that is, they kill tumor cells).
They are a cornerstone of precision medicine, a form of medicine that uses information about a person’s genes and proteins to prevent, diagnose, and treat disease. More than 300 companies worldwide are involved with developments focused on novel cancer therapies with a growing number focusing on specific cancer targets. There are over 200 novel cancer projects in phase III development, 400 projects in phase II development and 250 phase I projects. This shows that there remains a strong drop in the number of projects reaching phase III, about half of the projects reach this phase. This is not uncommon in any segment of drug or biological therapy development; however, it is always a concern for developers.
HOW ARE TARGETS IDENTIFIED?
Cancer genetics is the study of DNA sequence and gene expression differences between tumor cells and normal host cells. Several approaches exist to compare proteins, mutations, and chromosomal abnormalities in cancer cells and normal cells. These targets play a key role in cancer cell growth and survival, therefore, therapies that interfere with them can be viable cancer treatment option. Cancer genomics research is cutting edge and working to rapidly identify new targets. For example, researchers at the Institute for Cancer Research, London have discovered molecules that block the activity of two proteins that encourage the growth of cells in neuroblastoma. This discovery could transform the way that aggressive cancers are treated. Moreover, by understanding cancer cell biology researchers can identify new targets to combat deadly cancers, such as late-stage pancreatic cancer. A research group at the NIH has identified a signaling protein, leukemia inhibitory factor (LIF), as a key growth factor in tumor progression. This discovery has led to the initiation of a phase 1 clinical trial using monoclonal antibodies to block LIF signaling in pancreatic and other types of cancers.
HOW ARE THERAPIES DEVELOPED
As mentioned above, once a target has been identified, the next step is to develop a therapy, i.e. small molecules or monoclonal antibodies, which interferes with a cancer cell’s ability to grow and survival. Small molecules have low molecular weight so they can easily enter cells, therefore their targets are typically located within cancer cells. Once small molecule targets are determined by high-throughput screens, lead compounds and variations are tested for effectiveness on target with minimal effects on nontarget molecules. Monoclonal antibodies have relatively high molecular weight and generally cannot enter cells, so they are used for external targets. Monoclonal antibodies are developed by injecting animals with purified target proteins, which cause the animal to produce different antibodies against the target, which are then tested for binding affinity of target without binding non-target proteins. To prevent an antibody response against a foregin agent, human hybridomas are then produced using human myelomas that synthesize human monoclonal antibodies.
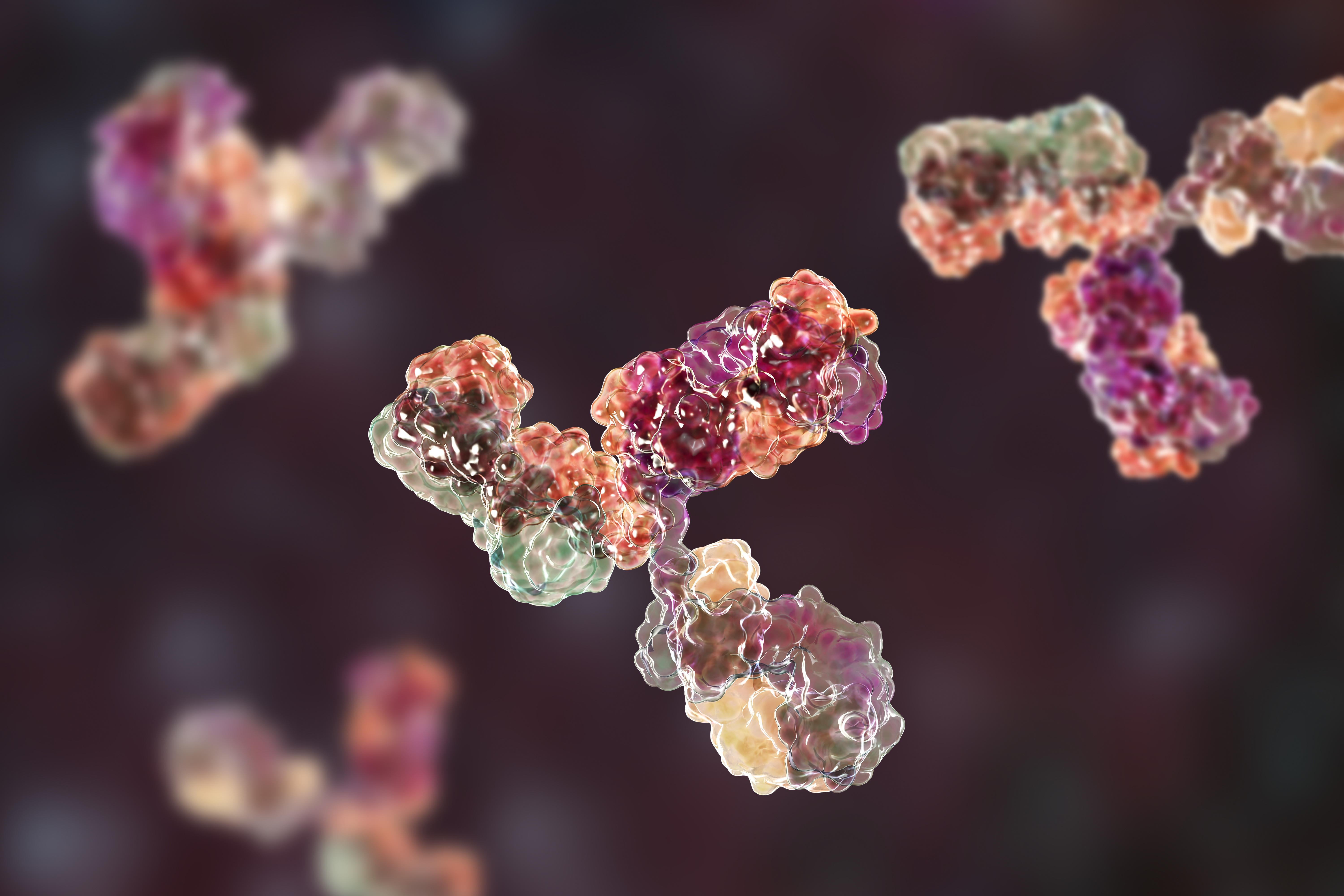
Monoclonal Antibodies
The use of monoclonal antibodies in cancer therapy is currently the subject of intense investigation. Human hybrids produce the single type of antibody molecule that they inherited from the normal, antibody-forming parent cell. Hybrid cells derived in this way can produce unlimited quantities of specific antibodies. These antibodies can be used to deliver a cytotoxic drug preferentially to the cancer cell and, thus, minimize drug interactions with normal cells. Similarly, antibodies can be used to direct other cytotoxic cells, such as macrophages and T cells, to tumor cells lurking in the body. Antibodies can be attached to a radioactive label and injected into a patient to screen for recurrence of tumor growth. Antibodies can also be directed against cells that support tumor growth. Due to the sensitivity of these treatments to the immune systems, researchers are developing innovative methods to reduce side effects for patients.
In 2019 alone, the FDA has already approved 17 different monoclonal antibody therapies to treat cancer. The global targeted cancer treatment market is estimated to be valued at $96.7 billion in 2017. The market increased at a compound annual rate of 14.5% from $32.6 billion in 2010 and is expected to reach $162.2 billion, showing 7.7% growth on average through 2025. So the markets and regulatory agencies are in agreement: targeted therapies will become increasingly important in the treatment of cancer. Our hope in science and society lies with these therapies and many others which are working together to beat cancer.
If you liked this article then you may be interested in some of our other content:
- Trends in Bioprocessing: Continuous Upstream Bioprocessing
- Oncologists Embrace the Liquid Biopsy for Precision Cancer Treatment
Copyright © 2019 scienceboard.net






