September 29, 2020 -- An unconventional subset of T cells may be strongly activated in patients with severe cases of COVID-19, according to a new study published in Science Immunology on September 28. This finding may lead to a new understanding of how the immune system responds to SARS-CoV-2 infection.
The balance between protective versus pathological immune responses in COVID-19 has been a concern since the onset of the pandemic. SARS-CoV-2 infection can lead to acute respiratory distress syndrome (ARDS), a condition characterized by aggressive inflammatory responses in the lower airways. The complex immune dysregulation of both innate and adaptive immune and inflammatory components has resulted in an unmet need to characterize COVID-19 immunopathogenesis.
"To find potential treatments against COVID-19, it is important to understand in detail how our immune system reacts and, in some cases, perhaps contribute to worsening the disease," said author Johan Sandberg, PhD, professor at the department of medicine, Huddinge, at Karolinska Institutet, in a statement.
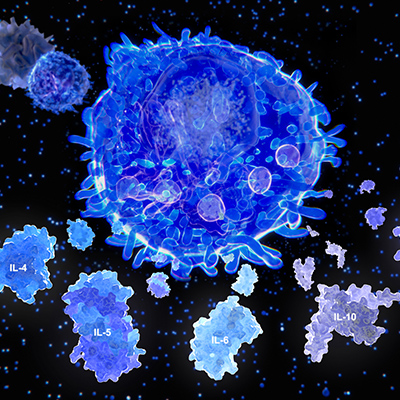
Most T cells play a role in CD8 and CD4 T-cell adaptive responses during COVID-19. However, the T-cell compartment also contains several unconventional T-cell subsets that have innate-like function.
For example, mucosa-associated invariant T (MAIT) cells make up 1% to 10% of T cells in circulation. MAIT cells are antimicrobial T cells that recognize bacterial metabolites and function as innate-like sensors and mediators of antiviral responses. Recent evidence has demonstrated that MAIT cells are activated in response to RNA viruses, namely HIV and influenza virus.
To determine the impact of these cells during SARS-CoV-2 infection, researchers from Karolinska Institutet investigated the MAIT cell compartment in COVID-19 patients with moderate and severe disease, as well as in convalescence. The team examined blood samples from 24 patients admitted to Karolinska University Hospital with COVID-19 disease and compared them to blood samples from 14 healthy controls and 45 individuals who had recovered from COVID-19.
The researchers found that the number of circulating MAIT cells was sharply lower in COVID-19 patients and the remaining MAIT cells were highly activated, indicating that they play a role in the response to SARS-CoV-2. Further, single-cell RNA sequencing data suggests that MAIT cells are highly enriched among T cells infiltrating in the airways of COVID-19 patients.
Flow cytometry phenotypes of MAIT cells in COVID-19 found that they were characterized by high expression of CD69 (CD69high) and diminished expression of the chemokine CXCR3 (CXCR3low). Both phenotypes were associated with poor clinical outcomes in the patient cohort. Within the airways, transcriptomic analysis revealed significant MAIT cell enrichment and proinflammatory interleukin 17A (IL-17A) profile.
"Taken together, these analyses indicate that the reduced number of MAIT cells in the blood of COVID-19 patients is at least partly due to increased accumulation in the airways," Sandberg said.
In convalescent patients, there seems to be a recovery of MAIT cells, including normalization of phenotypes, within weeks from resolution of symptoms. The authors suggested that this may help patients fight future microbial infections. Interestingly, CXCR3 levels were still low in some convalescent samples, raising the possibility that it may be a lasting alteration in MAIT cells post-COVID-19.
"The findings of our study show that the MAIT cells are highly engaged in the immunological response against COVID-19," Sandberg explained. "A likely interpretation is that the characteristics of MAIT cells make them engaged early on in both the systemic immune response and in the local immune response in the airways to which they are recruited from the blood by inflammatory signals. There, they are likely to contribute to the fast, innate immune response against the virus. In some people with COVID-19, the activation of MAIT cells becomes excessive and this correlates with severe disease."
Do you have a unique perspective on your research related to infectious diseases or virology? Contact the editor today to learn more.
Copyright © 2020 scienceboard.net