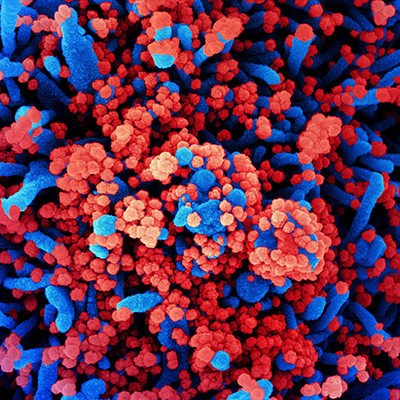
September 28, 2020 -- Monoclonal antibodies (mAbs) isolated from the blood of recovered COVID-19 patients -- known colloquially as "convalescent plasma" -- could be potentially useful as therapeutic and prophylactic agents for passive vaccination, assuming their administration does not trigger unwanted side effects. The findings of the new study were published in Cell on September 26.
Antibodies that target the receptor binding domain (RBD) of the SARS-CoV-2 viral spike protein S1 can compete with its binding to human angiotensin-converting enzyme 2 (ACE2) to prevent viral entry and subsequent infection. Ready-made antibodies, which are prepared from antibodies taken from plasma from a donor who recently had COVID-19, can be directly given to individuals as a means of passive vaccination.
This type of passive immunity is not as durable as active vaccination because the antibodies degrade over time. But passive vaccination has the benefit of being immediately effective, whereas active vaccination requires a building-up period.
Antibodies isolated from convalescent plasma of recovered COVID-19 patients carry low levels of somatic hypermutations, indicating limited affinity maturation and higher affinity antibodies, that make them attractive prophylactic or therapeutic agents. However, these near-germline mAbs can carry the risk of self-reactivity to autoantigens (self-proteins, DNA, or RNA).
Researchers from the German Center for Neurodegenerative Diseases (DZNE) and Charité - University Medicine Berlin selected 18 strongly neutralizing mAbs out of 598 antibodies drawn from the plasma of 10 COVID-19 patients by characterization of their biophysical properties, authentic SARS-CoV-2 neutralization, and exclusion of off-target binding in mice tissues. The antibody with the highest affinity, CV07-209, was also the strongest neutralizer of the virus in cell culture.
How do antibodies bind to the human receptor?
They solved the crystal structures of two neutralizing mAbs in complex with the RBD to demonstrate antibody engagement with ACE2. Using x-ray crystallography structures, the team characterized the mechanism of SARS-CoV-2 neutralization of the two mAbs, CV07-250 and CV07-270.
These represent antibodies encoded by different germline genes but that bind to the same epitope in the RBD. The different antibodies competed with ACE2 binding through steric hinderance, approaching the site through various angles and achieving various levels of epitope coverage.
Can SARS-CoV-2 antibodies bind to self-antigens?
During the investigation, the researchers examined reactivity of SARS-CoV-2 mAbs with unfixed murine tissues to determine whether the antibodies bind to self-antigens. They found that a fraction of SARS-CoV-2 neutralizing antibodies also bound to brain, lung, heart, kidney, or gut expressed epitopes. Reactivity with host antigens should be prevented, but complete exclusion of these antibodies can generate holes in the antibody repertoire. Whether these self-reactive antibodies can contribute to extra-pulmonary symptoms in COVID-19 remains to be seen.
"These antibodies bind not only to the virus, but also to proteins in the body that have nothing to do with the virus. Future research is needed to analyze whether the associated tissues could potentially become targets of attacks by the own immune system," said Dr. Harald Prüss, PhD, research group leader at the DZNE and also a senior physician at the Clinic for Neurology with Experimental Neurology at Charité - University Medicine Berlin, in a statement. "On the one hand, we need to be vigilant in order to detect any autoimmune reactions that may occur in the context of COVID-19 and vaccinations at an early stage. On the other hand, these findings can contribute to ensure the development of an even safer vaccine."
Antibodies for passive vaccination
The researchers selected mAb CV07-209 for its in vitro efficacy and absence of tissue-reactivity for in vivo evaluation. Systemic application with a single dose of CV07-209 in a hamster model of SARS-CoV-2 infection led to clinical improvement and reduced lung pathology, confirming the efficacy of prophylactic administration of mAbs. The researchers also found that post-exposure treatment in hamsters led to viral clearance, clinical remission and prevention of lung injury.
"Now, we are working with our industrial partner to establish the conditions that will allow for the most effective large-scale production of the antibodies we have identified," Prüss said. "The next step is clinical trials, that is testing in humans. However, this can not be expected before the end of this year at the earliest. The planning for this has already started."
Do you have a unique perspective on your research related to vaccine research? Contact the editor today to learn more.
Copyright © 2020 scienceboard.net