February 28, 2020 -- sing adeno-associated virus (AAV) technology, researchers have developed a novel gene therapy that can regenerate functional neurons in mouse models of Huntington's disease. The work was published in Nature Communications on February 27.
Huntington's disease (HD) is an autosomal-dominant disease that causes progressive motor, cognitive, and psychiatric symptoms associated with neuronal dysfunction and atrophy of the striatum. It is caused by an expanded chain of polyglutamines in the N-terminal region of the huntingtin protein (Htt) leading to intracellular accumulation and aggregation of mutant Htt (mHtt). This genetic change impacts GABAergic medium spiny neurons (MSNs), the most predominant type of neuron within the human striatum.
Recent strategies have used endogenous glial cells for neuroregeneration as a cell replacement therapy that minimizes immunorejection caused by foreign cells. Alternatively, researchers from Jinan University in China have successfully achieved in vivo direct reprogramming of adult glial cells into functional neurons in both astrocytes and NG2 cells. Next, they wanted to achieve this direct neuroregeneration in striatal cells as a potential therapy for HD.
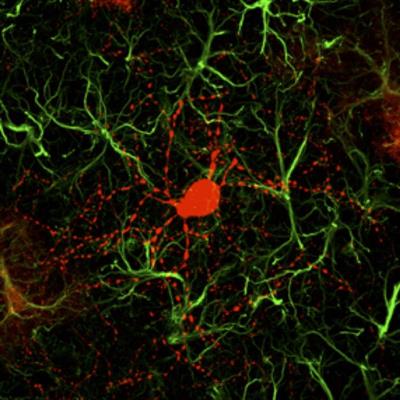
In the new study, a research team led by Gong Chen, PhD, achieved in vivo direct reprogramming of adult glial cells, nonelectrophysiologically functional cells that maintain homeostasis and protect neurons, into functional neurons. The researchers had previously shown that overexpressing neural transcription factors, such as neurogenic differentiation 1 (NeuroD1) in mouse brains promotes conversion of other types of brain cells into functional glutamatergic neurons.
So, to generate GABAergic neuron regeneration, the researchers designed a recombinant AAV vector that contained NeuroD1 and distal-less homeobox 2 (Dlx2), another transcription factor, which they injected into mice to drive expression of NeuroD1 or Dlx2 expression.
The researchers found that 80% of AAV-infected striatal cells were directly converted into GABAergic neurons. These neurons were electrophysiologically functional and formed synaptic circuits with other neurons. They also found that in vivo regeneration of GABAergic neurons in the striatum reduces the striatum atrophy and alleviates a series of phenotypic abnormalities, including the improvement of motor functions in the mouse model.
"The most exciting findings of this HD study are the significant motor functional recovery and remarkable extension of life span among the gene therapy-treated HD mice," said Chen, a former professor at Penn State University and current leader of a brain repair center at Jinan University, in a statement. "An ideal approach may be to combine our neuroregenerative approach together with gene correction technology to generate healthy new neurons in future studies."
Do you have a unique perspective on your research related to gene therapy or neurodegenerative disease research? Contact the editor today to learn more.
Copyright © 2020 scienceboard.net






