February 10, 2020 -- Researchers are using 3D models of human intestines -- a so-called "gut in a dish" -- to simulate leaky gut conditions, in which microbes and molecules seep out of the intestines. The research, published in Life Science Alliance on February 10, will help identify biomarkers for leaky gut for improved diagnostics and treatment development.
Leaky gut is a condition that occurs as a breakdown of tight junctions between cells in the gut lining. The body's largest immune system, the gut barrier, is the physical barrier that maintains homeostasis and protects the body from trillions of diverse microbes, antigens, and toxins. Compromised gut barriers may contribute to a variety of diseases, ranging from metabolic syndrome and chronic organ dysfunction to neurodegenerative diseases and even cancers.
The underlying mechanisms of how the gut barrier becomes compromised are largely unknown, but scientists do know that exposure to stressors may contribute to the problem. Stressors can cause cell-to-cell tight junctions to loosen due to loss of cell polarity, which is controlled by the stress-polarity signaling (SPS) pathway. This pathway is exclusively triggered in response to stress.
Previous studies have reported the importance of AMP-activated protein kinase (AMPK) in the maintenance of epithelial cell polarity and barrier functions in the context of stress. Specifically, GIV (Gα interacting, vesicle-associated protein), a multimodular polarity scaffold protein, is a substrate of AMPK and protects the epithelium by physically stabilizing tight junctions.
Despite this working molecular knowledge of the SPS pathway, clinicians do not have an easy way to diagnose leaky gut, lacking viable biomarkers for the condition. So, they used a near-physiologic model (cocultures of microbes with mouse and human organoids) to assess the importance of the SPS pathway in the gut barrier and explore the therapeutic potential of AMPK agonists, such as metformin, in strengthening the gut barrier
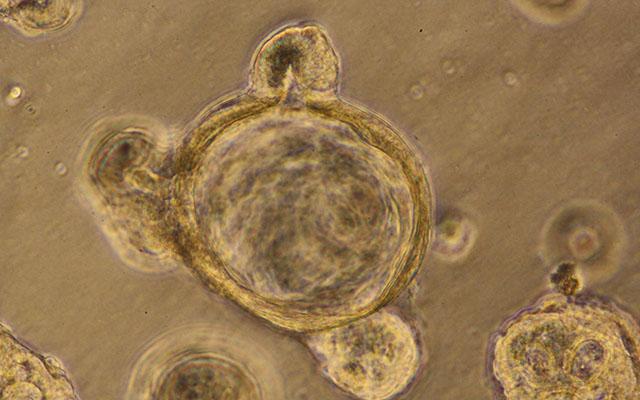
The researchers leveraged the tightly packed scutoid structure of the gut, where cells differentiate as they move from the bottom (crypt) toward the top (microvillus). The 3D "gut-in-a dish" model was built from crypt-derived stem cells isolated from human or mouse colons that differentiated into polarized enteriod-derived monolayers (EDMs). The EDMs contained enterocytes, goblet, Paneth, enteroendocrine, and tuft cells -- all cell types that are normally present in the gut lining. Moreover, they confirmed that the SPS pathway was active in the model.
Using EDMs, the scientists simulated a stress response by exposing the cells to Escherichia coli, lipopolysaccharide (LPS; toxic components of gram-negative bacteria), and hydrogen peroxide (induces oxidative stress). EDMs were assessed for gut barrier integrity via immunofluorescence staining of two biomarkers (pS245-GIV for the SPS pathway and occludin for tight junctions) and transepithelial electrical resistance (TEER). All of the stressors caused disruption in the barrier integrity.
But treatment with metformin preserved barrier integrity (tight junction maintenance) via increased occludin levels by as much as sixfold compared with untreated cells.
"Lots of research is done in mice that are inbred so that they are genetically identical, all in the same cage, eating the same diet, in order to remove these variables from the studies," said Dr. Pradipta Ghosh, professor of cellular and molecular medicine at the University of California (UC) San Diego School of Medicine and Moores Cancer Center, in a statement by the university. "But lab mice are far more standardized than the same human from day to day, or patients we see in the clinics. Here, our model is a better representation of humanity. On the other hand, it also means that each organoid is its own unique experiment. We have to test many organoids to be able to make any claim, which we did in our study."
Next, the researchers will take a closer look at the diseases driven by leaky gut. They also plan to test various ways to tighten junctions in the context of aging, inflammatory bowel disease, cancer, and other conditions to see if they can reduce or prevent initiation and progression of these diseases.
"I think you'd be hard-pressed to find a disease in which systemic inflammation is not a driver," said senior author Soumita Das, PhD, associate professor of pathology at UC San Diego School of Medicine. "That's why, even though there are so many things we still don't know, we're excited about the broad potential this model and these findings open for developing personalized leaky gut therapeutics that target AMPK and the stress-polarity signaling pathway."
Do you have a unique perspective on your research related to metabolic research, disease research, or pathology? Contact the editor today to learn more.
Copyright © 2020 scienceboard.net


